Candida auris: A Global Threat Hiding in Plain Sight -
Diagnostics, Resistance, and Clinical Fallout
Live Event: Thursday, January 15, 2026 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until July 15, 2026 | Florida Laboratory Credit
available |
|
Candida auris has emerged as a
globally significant multidrug-resistant fungal pathogen associated with
high morbidity, mortality, and substantial infection-control challenges.
Its ability to persist on environmental surfaces, cause
healthcare-associated outbreaks, and exhibit resistance to multiple
antifungal classes underscores the need for effective detection and
management strategies.
This webinar will review the clinical implications of C. auris
colonization and infection, highlighting the current understanding of
transmission dynamics, risk factors, and patient outcomes. We will
examine approaches to screening, including optimal body sites for
specimen collection, the role of targeted versus universal screening in
high-risk care settings, and the strengths and limitations of
culture-based and molecular diagnostic methods.
This webinar will:
•
Describe the clinical significance of C.
auris colonization and infection, including its epidemiology,
transmission pathways, associated patient outcomes, and implications for
healthcare systems
•
Evaluate current strategies for screening
and identifying C. auris colonization, comparing specimen
collection sites, culture-based methods, and molecular diagnostic
approaches
•
Interpret antifungal susceptibility testing
(AFST) results for C. auris, including awareness of
method-specific considerations, resistance patterns, and available
breakpoints or epidemiologic cutoff values
•
Apply laboratory findings to clinical and infection-prevention
decision-making, integrating screening results and AFST data into
patient management, outbreak containment, and facility-level control
strategies

|
Presenter:
Dr. Nathan Ledeboer
Professor of Pathology and Chief
Division of Clinical Pathology, Department of Pathology
Medical College of Wisconsin
Associate Chief Medical Officer for Laboratory Services
Froedtert Health

Dr. Nathan Ledeboer is the director of medical and technical
activities for the Clinical Microbiology and Molecular
Diagnostics Laboratories of the Medical College of
Wisconsin. In this role, he oversees development and
implementation of new assays and sign-out of all testing
performed in these laboratories. Ledeboer earned a PhD at
the University of Iowa, Carver College of Medicine,
completed fellowships at the Washington University School of
Medicine/Barnes-Jewish in St. Louis, and is board-certified
in medical microbiology.
|
Natural Disaster Preparedness in the Clinical Laboratory
Live Event: Wednesday, November 19, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until May 19, 2026 | Florida Laboratory Credit
available |
|
Help Mitigate or Minimize Disruption to Patient Care
Natural disasters impact communities and healthcare providers worldwide.
The challenges these events present for the clinical laboratory can lead
to risks in delivering quality patient care and meeting test turnaround
times that clinicians rely on for patient treatment decisions.
Understanding the vulnerabilities for your laboratory and having an
emergency preparedness plan that encompasses natural disaster response
is critical in mitigating or minimizing disruption to patient care.
These myriad challenges include everything from water quality concerns
to operating with interrupted connectivity to the laboratory or hospital
information systems. In the wake of a disaster, labs face operational
strain and inefficient testing workflows. For patients, it can mean
delayed treatment or sample recollections. At the institutional level,
this impacts everything from resource allocation to overall public
health response.
This webinar will provide attendees with actionable strategies for
addressing these challenges by using a natural disaster preparedness
plan. Featuring real-life natural disaster scenarios from three
laboratory leaders, the session will focus on how natural disasters can
impact any laboratory and how to proactively prepare for challenges.
This webinar will:
•
Discuss how natural disasters can impact
your clinical laboratory
•
Explain some applicable steps laboratory
personnel can take to be natural disaster-ready
•
Discover where to find resources to help your laboratory become more
prepared and ready to navigate challenges presented by natural disasters
 |
Presenters:
Moderator: Laura Osborne, MHSA, MLS(ASCP)CM
Sr. Marketing Manager, Clin Lab Systems & Assays,
QuidelOrtho North America Commercial Operations

Lacey Campbell, MHS, MLS (ASCP)
Chemistry Supervisor and Point of Care Coordinator
Springhill Medical Center

Trevor Davidson, MLS (ASCP)
Laboratory Supervisor
MyMichigan Health
 |
Transforming Care: The Strategic Shift to Value-Based Population
Health
Live Event: Wednesday, November 5, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until May 5, 2026 | Florida Laboratory Credit
available |
|
Join Emily Purvis from Baptist Health Pensacola as she shares her
organization’s journey adopting value-based care (VBC) and population
health strategies for diabetes management. She will outline why VBC
aligns with Baptist’s mission, the challenges that drove change, and how
proactive, patient-centered models are helping improve outcomes.
Emily will also highlight quality improvement initiatives, including how
point-of-care testing supports metrics such as the Merit-Based Incentive
Payment System (MIPS) and the Healthcare Effectiveness Data and
Information Set (HEDIS), and strengthens data capture for risk
adjustment scoring.
This webinar will:
•
Define quality management strategies for
diabetes care
•
Identify barriers and opportunities in
population health management
•
Apply approaches to help improve care
coordination and outcomes
•
Evaluate prevention-focused, patient-provider collaboration models

|
Presenter:
Emily Purvis
Population Health Program Manager
Baptist Health Care

Emily Purvis is a seasoned healthcare leader with a
background in medical coding and a passion for improving
care delivery through collaboration and innovation. As a
certified professional coder (CPC) and certified risk
adjustment coder (CRC), she brings expertise in value-based
care, regulatory compliance, and risk adjustment strategies. |
Pharmacogenomics: A Path to Precision Stroke and Cardiac Care
Live Event: Tuesday, October 7, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until Aril 7, 2026 | Florida Laboratory Credit
available |
|
Pharmacogenomics is playing an increasingly
vital role in cardiology and neurology, particularly in guiding
antiplatelet therapy for patients at risk of further complications from
minor strokes or other cerebrovascular events. This webinar will explore
the latest clinical evidence supporting the use of rapid CYP2C19-guided
antiplatelet therapy.
The session will highlight the practical aspects of implementing rapid
CYP2C19 genotyping in clinical practice. Presenters will share lessons
learned from real-world adoption, focusing on workflow integration,
clinical decision support, and the role of interdisciplinary
collaboration in ensuring effective use of genetic information for
neurologic patients.
In addition, the webinar will address the broader infrastructure needed
to support rapid genomic testing in lab and clinical environments.
Topics will include best practices for lab stewardship, integrating
genomic workflows, and leveraging electronic medical records (EMRs) to
surface actionable insights. Attendees will leave with strategies to
incorporate genomic data into clinical care pathways, supporting more
precise, data-driven decisions for prevention and treatment.
This webinar will:
•
Evaluate current clinical evidence supporting CYP2C19-guided
antiplatelet therapy and its impact on patient outcomes
•
Examine the implementation and clinical use of rapid CYP2C19 genotyping
at MedStar Health to guide personalized antiplatelet therapy
•
Interpret key considerations for implementing genomic testing in the
lab, including best practices for lab stewardship and integration into
existing workflows
•
Discover how to leverage your EMR to surface and act on genomic
insights, supporting clinical decision-making and enhancing patient care
 |
Presenters:
Max Smith, PharmD, BCPS
Georgetown University Hospital, Washington, DC

Dr. Max Smith is a clinical pharmacogenomics
specialist at MedStar Health and an assistant
professor at Georgetown University Medical Center.
Dr. Smith earned a PharmD at the University of
Toledo and is a board-certified pharmacotherapy
specialist. |
|
Amanda Hanson BS, MS, ASCP(MB)CM
Spartan Regional Healthcare System Spartanburg,
South Carolina

Amanda Hanson is a dedicated healthcare director
with over a decade of experience in clinical
laboratory management, and a unique blend of
expertise in precision medicine and community
health. Throughout her career, Ms. Hanson has
developed and implemented innovative solutions that
enhance patient care and operational efficiency. |
|
Advancing MPN Genomic Profiling with an Amplicon-Based Myeloid
NGS Panel
Live Event: Tuesday, September 30, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until March 30, 2026 | Florida Laboratory Credit
available
|
|
Myeloproliferative neoplasms (MPNs) are a
group of myeloid malignancies characterized by excessive production of
mature myeloid cells in the blood. Traditionally, labs use sequential
single gene testing (SGT) to evaluate somatic mutations in three driver
genes (JAK2, MPL, CALR), then pivot to next-generation sequencing (NGS)
if no mutations are found. However, this method is becoming inefficient
as the list of clinically significant biomarkers increases.
In this webinar, Dr. Krishnamurthy will share her experience with an
amplicon-based myeloid NGS panel for comprehensive genomic profiling of
MPNs. It provides a comprehensive assessment of driver genes (JAK2, MPL,
CALR, CSF3R) and other MPN-related genes with important prognostic and
therapeutic implications.
She will compare the myeloid NGS panel to the traditional PCR-based
sequential SGT, highlighting the benefits and limitations of both
approaches. Additionally, she will emphasize the need to reassess
traditional testing approaches to improve diagnostic accuracy,
prognostic evaluation, and therapeutic strategies.
This webinar will:
•
Describe the molecular profiling of MPN, including classification and
biomarkers implicated in the diagnosis, prognosis, and therapeutic
selection for MPN patients
•
Assess traditional sequential single genes testing via PCR in
identifying driver genes
•
Evaluate clinical scenarios where an amplicon-based myeloid NGS panel
identified critical co-mutations of clinical significance
•
Investigate a proposed diagnostic algorithm that integrates both PCR and
NGS for detecting very low variant allele frequencies (VAF) in driver
genes

|
Presenter:
Kritika Krishnamurthy, MD
Assistant Professor of Pathology
Albert Einstein College of Medicine |
 |
|
Dr. Krishnamurthy is an attending surgical pathologist,
hematopathologist, and molecular pathologist at Montefiore
Medical Center, Bronx, NY, and an assistant professor of
pathology at Albert Einstein College of Medicine. She also
holds the position of associate director for Molecular
Genetic Pathology and Cytogenetics Lab, and associate
program director for Molecular Genetic Pathology and
Laboratory Genetics and Genomics Fellowships at Montefiore
Medical Center. |
resenter:
|
The Role of hsTnI Algorithms at Outpatient Point-of-Care Sites
Live Event: Wednesday, September 24, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until March 24, 2026 | Florida Laboratory Credit
available |
|
Chest pain remains one of the most common and
challenging symptoms encountered in emergency departments (EDs).
Traditional evaluation pathways often result in unnecessary admissions,
extensive testing, and delayed decision-making. With the advent of
high-sensitivity troponin I (hsTnI) assays, clinicians can now more
confidently rule out acute myocardial infarction (AMI) and safely
discharge low-risk patients—helping to enhance both patient care and
departmental efficiency.
In this webinar, Dr. James McCord, an experienced cardiologist and
thought leader in cardiac diagnostics, will discuss how hsTnI testing at
the point of care is transforming risk stratification in both hospital
and outpatient environments. Using real-world examples and clinical
insights, he will address common misconceptions, serial testing
strategies, and how POC access to hsTnI can support decision-making in
freestanding EDs and urgent care centers.
This webinar will:
•
Discuss the clinical impact of
high-sensitivity troponin I (hsTnI) in emergency care settings
•
Identify how hsTnI supports efficient and
safe discharge decisions, especially in resource-limited environments
•
Discover the utility of hsTnI testing at the
point of care in freestanding EDs and urgent care
•
Recognize implementation challenges and
strategies to maintain consistency between POC and central lab testing
 |
Presenter:
James McCord, MD
Professor of Medicine
Wayne State School of Medicine

Dr. James McCord is a professor
of medicine at the Wayne State School of Medicine in
Detroit, MI. He currently serves as the associate program
director for cardiology research. His area of clinical
research includes cardiac biomarkers and the assessment of
patients in the emergency department for possible acute
coronary syndrome and heart failure. |
Easing Your Transformation to a Digital Workflow
Live Event: Wednesday, September 17, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until March 17, 2026 | Florida Laboratory Credit
available |
|
Many factors can impact the success of laboratories who are moving
toward digital-pathology-driven workflows. By understanding these
factors, laboratories can better optimize their digital workflows to get
the most out of their investments.
Anytime a new technology is added to a laboratory’s workflow, it can
present unforeseen challenges to its processes. These challenges can
range from quality-related issues to uncertainty in workflow continuity,
among others. By understanding these potential barriers early,
laboratories can help the digital transformation project progress
smoothly.
In this webinar, Dr. Eloy will identify the potential workflow
challenges of adopting digital processes and help participants learn how
to overcome obstacles by focusing on the right pre-analytical and
diagnostic workflow steps.
This webinar will:
•
Recognize the pre-analytic steps that impact digital workflows
•
Describe the diagnostic steps and challenges to implementing digital
workflows
•
Explain
process improvements that can be made to optimize your digital workflow
•
Discuss
how the use of digital processes and AI can help you improve efficiency

|
Presenter:
Catarina Eloy, MD, PhD
Director, Institute of Molecular Pathology and Immunology
University of Porto
Porto, Portugal

Dr. Catarina Eloy is a pathologist and Director of The
Institute of Molecular Pathology and Immunology of the
University of Porto (IPATIMUP). She joins BTS to discuss the
transformation of IPATIMUP to a fully integrated digital
pathology laboratory and how new technology is improving
diagnostic efficiency and patient treatment outcomes in
Portugal. Additional topics include AI initiatives for
pathology and advice on how to get started going digital. |
Accelerating Diagnosis and Enhancing Respiratory Disease
Management
Live Event: Tuesday, September 9, 2025 |
12:00 - 1:00 PM ET
P.A.C.E.®
credit available until March 9, 2026 | Florida Laboratory Credit
available |
|
Join us for an exciting webinar led by Dr. Amesh Adalja—an expert in
respiratory disease and point-of-care testing—who will discuss how rapid
antigen tests are impacting the diagnosis and management of respiratory
diseases in urgent and primary care settings. Discover how these tests
are affecting time to diagnosis, treatment outcomes, and patient care.
This webinar will:
•
Identify the advantages of rapid antigen testing for
respiratory diseases in urgent and primary care settings, including
speed and accuracy in diagnosis.
•
Examine case studies and real-world examples that demonstrate
the positive impact of rapid antigen testing on patient outcomes in
urgent and primary care.
• Describe ways to effectively integrate rapid antigen
testing into urgent and primary care practices to enhance overall
respiratory disease management and improve healthcare efficiency.
 |
Presenter:
Amesh A. Adalja MD FIDSA
FACP FACEP
Senior Scholar
Johns Hopkins Center for Health Security

Dr. Amesh Adalja is an infectious disease physician and
Senior Scholar at the Johns Hopkins Center for Health
Security. He is also Adjunct Assistant Professor at the
Johns Hopkins Bloomberg School of Public Health and an
Affiliate of the Johns Hopkins Center for Global Health. Dr.
Adalja’s work is focused in emerging infectious diseases,
pandemic preparedness, and biosecurity. He is a native of
Butler, Pennsylvania, and actively practices infectious
disease, critical care, and emergency medicine in the
Pittsburgh metropolitan area. |
Breathe Easy: The Power of Timely Testing in Respiratory Care
Live Event: Tuesday, August 5, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until February 5, 2026 | Florida Laboratory Credit
available |
|
Respiratory season presents a recurring challenge for healthcare
providers, with SARS-CoV-2, influenza, and RSV often circulating
simultaneously. During periods of high patient volume and overlapping
symptoms, it becomes increasingly difficult to differentiate between
infections based on clinical presentation alone.Learn strategies for
addressing respiratory diagnostic challenges and differentiating between
viruses using rapid antigen testing—particularly within the early
symptomatic window—to help improve patient care and drive operational
efficiency.
This webinar will:
•
Examine the clinical importance of early testing for SARS-CoV-2 and
influenza
•
Evaluate the role of rapid antigen testing within diverse care settings
•
Differentiate between molecular and antigen testing options based on
clinical need
•
Apply real-world insights from expert-led case examples and
implementation strategies
 |
Presenter:
Paul K Drain, MD, MPH
Associate Professor, Infectious Disease Physician,
Harborview Medical Center
University of Washington Medical Center

Dr. Paul Drain is Associate Professor in the Departments of
Global Health, Medicine (Infectious Diseases), and
Epidemiology at the University of Washington and a
practicing Infectious Disease physician at Harborview
Medical Center at the University of Washington Medical
Center in Seattle. His research group focuses on
development, evaluation and implementation of diagnostic
testing and clinic-based screening, including novel
point-of-care technologies, to improve clinical care and
patient-centered outcomes. |
Behind the Guidelines: H. pylori Management in 2025
Live Event: Tuesday, June 24, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until December 24, 2025 | Florida Laboratory Credit
available |
|
Helicobacter pylori (H. pylori) infection poses substantial
challenges in clinical practice; many patients remain undiagnosed or are
tested inadequately or receive inadequate treatment regimens that are no
longer recommended. The 2024 American College of Gastroenterology (ACG)
clinical guidelines have updated recommendations on the appropriate
diagnostic testing for and treatment of H. pylori infection.
However, many healthcare providers may still rely on older testing
methods or ineffective treatments. These knowledge and practice gaps
inevitably lead to suboptimal outcomes including persistence of H.
pylori infection, increasing antimicrobial resistance rates, and
increased healthcare costs.
This webinar, led by Dr. Steven F. Moss and Dr. Colin W. Howden, will
provide attendees with the latest updates from the ACG clinical
guidelines on H. pylori infection. Through an expert-led
discussion on who, when and how to test, the session will equip
healthcare providers and laboratory professionals with the knowledge to
apply the most effective diagnostic and treatment strategies. By
implementing the recommended Test-Treat-Retest approach, participants
will be able to enhance patient outcomes, avoid ineffective treatment
regimens, and ultimately improve institutional efficiency.
This webinar will:
•
Examine the epidemiology of H. pylori infection, including
prevalence and risk factors
•
Discuss the disease associations of H. pylori infection and its
recognized long-term consequences if left untreated
•
Discuss the ACG 2024 clinical guidelines on who should be tested for
H. pylori, with a focus on specific populations at risk of gastric
cancer
•
Review non-invasive testing methods and updated treatment protocols,
including the importance of universal re-testing after treatment
•
Explore strategies for managing patients in whom initial treatment has
failed with a consideration of the role of antibiotic resistance by
H. pylori

|
Presenters:
Colin W. Howden, MD
University of Tennessee Health Science Center, Memphis, TN

Dr. Howden has been a Professor of Medicine at the
University of South Carolina, Rush University, and
Northwestern University Feinberg School of Medicine. From
2014 to 2021, he served as the Hyman Professor of Medicine
and Chief of the Division of Gastroenterology at the
University of Tennessee Health Science Center.
Steven F. Moss, MD
Brown University, Providence RI

Dr. Steven Moss currently serves as a Professor of Medicine
and the Program Director of the Gastroenterology Fellowship
Training Program at Brown University, as well as the
Director of Endoscopy at Providence VA Medical Center. |
Utilizing Natriuretic Peptide Testing to Identify and Manage
Heart Failure
Live Event: Tuesday, May 27, 2025 |
2:00 - 3:00 PM ET
P.A.C.E.®
credit available until November 27, 2025 | Florida Laboratory Credit
available |
|
Heart failure is a growing issue in the U.S., with nearly 6.7 million
adults affected, a number expected to rise to 8.5 million by 2030. This
increase in prevalence presents a significant challenge for patients,
impacting their quality of life and healthcare institutions by
increasing the burden on resources.
This webinar will address these concerns by providing valuable insights
into the latest treatments and strategies for managing heart failure.
Attendees will gain knowledge to improve patient outcomes, reduce
healthcare strain, and enhance their clinical practices in managing
heart failure effectively.
This webinar will:
•
Explain how BNP levels reflect the heart's
function and how they can be used to identify patients at risk of
developing heart failure
•
Discuss the role of BNP in diagnosing and
risk-stratifying patients with heart failure, and in guiding their
management
•
Review the interplay between diabetes and heart failure, and how
natriuretic peptides can aid implementation of guideline-directed
therapies in heart failure and diabetes

|
Presenter:
Lori B. Daniels, MD, MAS, FACC, FAHA
Professor of Medicine
Director, Cardiovascular Intensive Care Unit
Sulpizio Cardiovascular Center, UC San Diego

Lori B. Daniels, MD, is a board-certified cardiologist and a
professor of medicine with the University of California, San
Diego, School of Medicine. She works with patients on the
prevention of cardiovascular disease and the management of
coronary disease, hypertension, hypercholesterolemia, and
other cardiovascular problems. Dr. Daniels believes good
communication with her patients is an important part of the
physician-patient relationship and strives to provide
evidence-based, yet individualized care to each one.
|
Helping Ensure Workflow Accuracy: Labeling, Tracking, and
High-Quality Slides
Live Event: Thursday, May 15, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until November 15, 2025 | Florida Laboratory Credit
available |
|
For lab professionals and pathologists,
keeping tissue samples intact throughout processing is crucial for
accurate diagnoses. Poor-quality adhesive slides can result in tissue
detachment, leading to inconclusive or erroneous assessments. And
without a reliable labeling system and high-performance materials, labs
face rework, wasted resources, and reduced confidence in results,
ultimately affecting both workflow efficiency and patient outcomes.
This webinar will highlight the importance
of using adhesive slides that maintain tissue integrity, so specimens
remain intact for precise and confident assessments. Additionally, the
session will provide critical insights into how on-demand printing can
significantly reduce labeling and tracking errors, enhancing overall
laboratory accuracy and efficiency. Attendees will learn about the
advantages of a validated printer and consumable ecosystem that delivers
consistent, high-performance results. By implementing these best
practices, institutions can reduce the likelihood of errors, optimize
workflows, and ultimately enhance patient outcomes.
This webinar will:
•
Discuss how on-demand printing offers better
patient safety
•
Identify the steps for moving from batch to
on demand printing
•
Describe the performance benefits of using
validated consumables with printers
•
Explain why slide adhesion is so important
 |
Presenters:
Rachel Finn, MBA, HTL (ASCP)CM
Product Marketing Specialist
StatLab Medical Products

Arielle Hobson
StatLab Product Manager,
Slides and Stains

Bill Martin
StatLab Product Manager,
Printers and Software

|
A Warning About Warning Rules
Live Event: Thursday, May 1, 2025 |
2:00 - 3:00 PM ET
P.A.C.E.®
credit available until November 1, 2025 | Florida Laboratory Credit
available |
|
Are QC Warning Rules still Relevant?
The 2s warning rule of the 1981 Westgard Rules has dictated the warning
rule of quality control (QC) for more than 40 years. After all this
time, do laboratories still need the warning? While the warning rule has
become a firmly entrenched tradition, does the science behind it still
hold up? Or are laboratories warning themselves to distraction?
This webinar will explore how QC has evolved in the last 44 years, how
the needs of the 20th century are different than what current
laboratories require, and how to objectively determine how much QC is
needed for any particular method.
This webinar will:
•
Describe the original Westgard rules, as
well as the updated Westgard Sigma Rules
•
Examine the analytical sigma metric and how
it identifies the risk of method failures and provides guidance on
optimal QC rule implementation
•
Illustrate where old warnings and new CLIA
requirements meet
•
Identify other common ways in which labs get the Westgard Rules wrong

|
Presenter:
Sten Westgard, MS
Director of Client Services and Technology
Westgard QC, Inc.

Sten Westgard is the director of client services and
technology for Westgard QC, Inc. For over 30 years, Westgard
has been managing Westgard Web, publishing, training, and
writing hundreds of reports, essays, and applications on
quality control, method validation, Six Sigma, and other
laboratory management topics.
|
Optimizing Chest Pain Care: Implementing Rapid Point-of-Care
Cardiovascular Diagnostic Testing into Your Workflow
Live Event: Thursday, April 17, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until October 17, 2025 | Florida Laboratory Credit
available |
|
Chest pain is a common presentation to the emergency department and the
most common reason for observation hospital admissions. Providers caring
for patients with acute chest pain must determine whether the patient
has acute coronary syndrome (ACS) or another life-threatening condition
associated with high mortality, morbidity, and malpractice risk.
Fear of missing these conditions leads many providers to over-test
patients with chest pain, costing over $13 billion each year and
crowding emergency departments and hospital wards. However, it is
estimated that 2% to 4% of patients with ACS are initially missed, which
can be due to an atypical presentation that leads to under-testing.
This webinar will discuss approaches to improve chest pain risk
stratification using point-of-care diagnostics. Specifically, we will
discuss high-sensitivity troponin, D-dimer, and natriuretic peptide
biomarker testing and the advantages of point-of-care testing. This will
include discussion of evidence-based algorithms that can be used to
integrate these point-of-care biomarkers into the emergency department
workflow.
This webinar will:
•
Identify the current challenges and
inefficiencies of emergency department chest pain risk stratification
•
Discuss how cardiovascular point of care
diagnostics can improve chest pain care
•
Describe the advantages of point of care
high sensitivity troponin and considerations for how best to implement
them into emergency department workflow
•
Analyze the utility of point of care D-dimer and natriuretic peptide
testing

|
Presenter:
Simon A. Mahler MD, MS, FACEP
Professor and Vice Chair of Research, Department of
Emergency Medicine
Professor of Epidemiology and Prevention
Professor of Implementation Science
Wake Forest University School of Medicine

Dr. Mahler is a Professor and Vice Chair of Clinical
Research for the Department of Emergency Medicine at the
Wake Forest School of Medicine. He completed a Master of
Science in Clinical and Population Translational Sciences at
Wake Forest University and a T-32 mentored research program
in Quality Care and Outcomes Research in Cardiovascular
Disease. |
H&E Staining: Science and Troubleshooting
Live Event: Wednesday, March 26, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until September 26, 2025 | Florida Laboratory Credit
available |
|
In this webinar, you’ll learn why routine hematoxylin and eosin (H&E)
staining is necessary and how chemical attractions are used for the
processes. You’ll also take an in-depth look at H&E staining methods,
exploring each critical step and the science behind them. Find out why
the steps are important for quality and efficiency and what could go
wrong if they are not executed properly. The presenter will also explain
the amazing history of one of the dyes that has been in use for 500
years. Lastly, he’ll provide examples of well-stained tissues and
bulletproof protocols.
This webinar will:
•
Discuss staining pathway steps
•
Explain the function of each staining step
in that pathway
•
Discover different staining methods
•
Examine ways to avoid common mistakes and correctly troubleshoot

|
Presenter:
Andrew Lisowski M.S., HTL (ASCP)
Senior Technical Content Manager
Epredia

A senior technical content manager at Epredia, Andrew
Lisowski has nearly 30 years of experience in histology and
histotechnology. He attended veterinary school and earned
his master’s degree in molecular biology. |
Using Telepathology to Advance Patient Care and Lab Workflow
Live Event: Thursday, March 20, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until September 20, 2025 | Florida Laboratory Credit
available |
|
Shortages in pathologists and lab staff are impacting support for
intraoperative frozen section (IFS) consultation and rapid on-site
evaluation (ROSE). Historically IFS and ROSE have required a
pathologist’s physical presence in the location where samples are being
prepared. This webinar will examine how telepathology and whole slide
imaging have advanced to a point where they can be used to convert
support of IFS and ROSE from on-site to remote.
This webinar will:
•
Identify the challenges presented for IFS
and ROSE procedures due to shortages of qualified pathologists and lab
staff
•
Discover how whole slide imaging (WSI)
enables remote diagnostics for IFS
•
Examine how WSI enables remote diagnostics
for ROSE
•
Evaluate specific technology to enable remote diagnosis for IFS and ROSE
 |
Presenters:
Hannah Krigman, MD
Professor of Pathology
Washington University St. Louis School of Medicine

Dylan Miller, MD
Professor of Pathology
University of Utah School of Medicine
 |
Antimicrobial Stewardship and the Impact of MICs on Patient
Outcomes
Live Event: Wednesday, January 29, 2025 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until July 29, 2025 | Florida Laboratory Credit
available |
|
Antimicrobial resistance continues to be a significant global health
threat. Delayed or inaccurate lab results could not only contribute to
the further development of resistance but could lead to the mistreatment
and potential mortality of patients with multi-drug-resistant
infections. The lack of successful antimicrobial and diagnostic
stewardship programs can exacerbate the overuse of broad-spectrum and
toxic antibiotics. Limited access to diagnostics that can deliver
accurate minimum inhibitory concentration (MIC) results for highly
effective new-generation drugs can lead to failed therapy, adverse
effects, increased costs, and increased potential for patient mortality.
The webinar will review the positive impact effective antimicrobial
stewardship can have on managing the development of resistance. The
presenter will also discuss how dosing new drugs based on accurate MIC
data can help reduce costs and improve patient outcomes.
This webinar will:
•
Examine the ways in which antibiotic stewardship can help healthcare
providers deliver optimal care and reduce unnecessary antibiotic
exposure risk
•
Explain how using institutional data can guide empiric therapy for
multi-drug-resistant infections
•
Discuss the importance of receiving timely and accurate organism
identification and susceptibility data when conducting daily antibiotic
stewardship activities and treating aggressive, complicated infections
•
Describe how effective stewardship can reduce the development of
resistance and improve patient outcomes

|
Presenter:
Jerod Nagel, PharmD, BCIDP
Clinical Pharmacist, Infectious Diseases Clinical Assistant
Professor, Director Infectious Disease Residency University
of Michigan Health Systems

Dr. Nagel has served as a leader for several organizations,
including the Antimicrobial Stewardship in Cancer
Consortium; the antimicrobial subcommittee of the Infectious
Disease Society of America; and the Vizient Antimicrobial
Stewardship committee. He has also been named the Society of
Infectious Disease Pharmacists Clinician of the Year. |
Optimizing Diagnostic Testing with Quality Controls and
Temperature Monitoring
Live Event: Tuesday, December 10, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until June 10, 2025 | Florida Laboratory Credit
available |
|
Molecular diagnostics are an integral tool in the detection of
infectious diseases. Despite dramatic advances in laboratory technology,
many patients continue to receive inaccurate, incomplete, or delayed
diagnoses. Clinical laboratories performing infectious disease testing
are challenged to improve test performance and patient-sample
temperature monitoring to decrease testing errors and enhance diagnostic
speed and accuracy.
In this webinar, you’ll learn how quality controls offer a productive
method for identifying, evaluating, and correcting testing flaws due to
system failure, environmental conditions, or operator performance -
before results are reported. We’ll also discuss quality controls’
ability to help fulfill regulatory requirements and examine the role of
temperature measurement and monitoring instruments in safeguarding
patient samples.
This webinar will:
•
Assess the critical role of quality controls
•
Identify attributes of effective quality
controls
•
Evaluate quality control solutions for
clinical laboratories
•
Apply certified measurement and monitoring instruments
 |
Presenters:
Cindy Gisler
Product Manager at Traceable

Ms. Gisler holds a BS in Medical Technology from the
University of Texas Medical Branch and a BA in Biology from
Trinity University.
Jessica Van Allen, PhD Technical Support
Lead at ZeptoMetrix

Dr. Van Allen received her BS in Chemistry from Nazareth
College and her PhD in Biochemistry from the University of
Rochester. |
A Practical Approach to Managing Cardiovascular-Kidney-Metabolic
Syndrome
Live Event: Tuesday, December 3, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until June 3, 2025 | Florida Laboratory Credit
available |
|
Cardiovascular-kidney-metabolic (CKM) syndrome is an emerging and
critical health concern due to its high prevalence and association with
chronic kidney disease (CKD) and cardiovascular events. In this webinar,
we’ll focus on identifying individuals at high risk for CKD by utilizing
estimated glomerular filtration rate (eGFR) and albumin-to-creatinine
ratio (ACR) testing to achieve accurate risk stratification.
You’ll learn how to employ risk stratification techniques, including CKD
heatmaps, to predict kidney and cardiovascular outcomes. This approach
facilitates targeted patient education and guides individualized
interventions for kidney and cardioprotection. We’ll also define
essential roles within primary care and nephrology and highlight
practical strategies for implementing CKM-focused screening and
management in routine practice.
This webinar will:
•
Discuss the detection and
risk-stratification of CKD with eGFR and ACR testing
•
Assess kidney and cardiovascular risk using
heatmaps and prediction equations
•
Evaluate patient education and guide kidney
and cardioprotective interventions
•
Examine the Integration of CKM-focused screening and management into
routine practice

|
Presenter:
Joseph A. Vassalotti, MD
Clinical Professor
Icahn School of Medicine at Mount Sinai

Dr. Vassalottii has led collaborations to develop the Kidney
Health Evaluation for Adults with Diabetes quality measure
to improve evidence-based CKD testing with eGFR and
albuminuria and guide detection, risk stratification, and
interventions proportional to risk. He has served as
principal investigator for an AARP-funded Quality Measures
Innovation Grant to analyze CKD testing interactions with
detection, evidence-based interventions, and health equity.
He is also a co-investigator for the Centers for Disease
Control and Prevention's (CDC) CKD Surveillance Project. |
The Microbiology Lab’s Role in Managing Critical Cases
Live Event: Thursday, October 31, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until May 1, 2025 | Florida Laboratory Credit
available |
|
How accurate MIC results can help manage critical patients with
multidrug-resistant organism infections
The microbiology laboratory plays a critical role in the acute
management of patients. The selection of the method to determine
Antimicrobial Susceptibility results and specifically MIC’s is crucial.
It is of particular significance in determining the appropriate
treatment for critically ill patients with severe infections. The
knowledge of and extended capacity for testing novel antimicrobial
agents is of specific importance. Delayed or inaccurate results can lead
to the mistreatment, complications with and the potential mortality of
patients with multi-drug resistant infections.
Empiric therapy may be inappropriate due to a lack of treatment options.
Toxic drugs like Colistin and Vancomycin are often used encouraging
spread of resistance and complications. Antimicrobial Stewardship Teams
are in place to help implement more effective strategies, but in the
absence of a diagnostic tool that provides accurate MIC data guiding
treatment options, poor practice can persist. The inability to identify
effective treatment options including those involving new generation
antimicrobials can have a devastating impact on patient outcomes.
We will review three challenging cases where critically ill patients
illustrating the role the microbiology lab plays in management of
critical cases. The knowledge of and having the capacity to test new
antimicrobial agents can have a significant impact on the patient
outcomes when dealing with multi-drug resistant infections.
This webinar will:
•
Restate the importance of the correct antibiotic selection for
critically ill patients and the risk of poor outcomes
•
Discuss the utility of multiple data sources including antibiograms and
combination antibiograms in the selection of effective treatment options
•
Describe the ways in which new generation therapeutics and accurate MIC
results can help manage critical patients
•
Explain the importance of accurate results and breakpoints when treating
critically ill patients

|
Presenter:
James A. McKinnell, MD
Associate Professor of Medicine
David Geffen School of Medicine
University of California, Los Angeles
Division of Infectious Disease LA-Biomed at Harbor UCLA
Medical Center
Dr. James McKinnell is an Associate Professor of Medicine at
the David Geffen School of Medicine at the University of
California, Los Angeles. He is also a member of the
Infectious Disease Clinical Outcome Research Unit (ID-CORE)
and the Los Angeles Biomedical Research Institute at
Harbor-UCLA. He is a nationally recognized infectious
disease specialist with specific research interests related
to the clinical management and prevention of
healthcare-associated infections. He has published over 40
papers, many with emphasis on optimal use of antibiotics and
antimicrobial resistance within the community. |
Preparing Your Laboratory for the CLIA 2024 Proficiency Testing
Changes
Live Event: Wednesday, October 23, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 23, 2025 | Florida Laboratory Credit
available |
|
Revisions to the Clinical Laboratory Improvement Amendments (CLIA)
proficiency testing regulations that went into effect on July 11, 2024,
are driving change in today’s labs. The updates include 29 newly
regulated analytes and tighter proficiency testing acceptable limits for
many currently regulated analytes - along with changes to grading and
reporting.
In this webinar, we’ll examine these shifts more closely and determine
actionable steps laboratorians can take to comply. We'll also discuss
the essentials of proficiency testing and how to avoid noncompliance
during CLIA inspections. Plus, we will address your specific needs with
a Q&A session following the presentation.
This webinar will:
•
Summarize the historical aspects and other provisions of the CLIA
Proficiency Testing Final Rule
•
Describe the finalized CLIA requirements pertaining to clinical
chemistry and immunoassays, including acceptable limits and total
allowable error
•
Discuss applicable steps laboratorians can take to adhere to CLIA
regulatory changes
•
Apply essential best practices to avoid noncompliance in proficiency
testing and CLIA inspections
 |
Presenter:
Bremansu Osa-Andrews, PhD, DABCC, NRCC
Clinical Assistant Professor of Pathology, Immunology, and
Laboratory Medicine; Medical Director of Core Lab Chemistry,
Urinalysis, and Immunology; and Medical Director of the
Endocrinology Lab at the University of Florida

Dr. Bremansu Osa-Andrews is a board-certified clinical
chemist-diplomate of the American Board of Clinical
Chemistry (ABCC) and the National Registry of Certified
Chemists (NRCC). As an experienced College of American
Pathologists (CAP) inspector, he has a profound
understanding of CAP/CLIA standards and requirements for
clinical laboratories, along with a background in quality
assurance, quality control, and regulatory compliance. |
Generating Flawless Slides for Digital Pathology
Live Event: Thursday, October 17, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 17, 2025 | Florida Laboratory Credit
available |
|
Improperly prepared stained slide sections can lead to delays and higher
costs in histology labs. Learn how you can find, fix, and avoid workflow
errors to produce slides that help improve scanning efficiency, shorten
turnaround times, and accelerate accurate diagnoses.
This webinar will:
•
Recognize challenges that affect stained
section quality
•
Identify issues associated with the
embedding and sectioning workflow steps
•
Evaluate detailed examples of glass slides
that create scanning problems
•
Apply best practices for printing scannable barcodes

|
Presenter:
Andrew Lisowski, MS, HTL(ASCP)
Senior Technical Content Manager
Epredia

Andrew Lisowski has nearly 30 years of experience in
histology and histotechnology. He attended veterinary school
and earned his master’s degree in molecular biology. He has
worked in histology, IHC and ISH labs, cell culture lab,
performed in-vitro and in-vivo toxicology assays, and was a
member of a necropsy team.
|
Amplicon-Based Semiconductor Sequencing in Biomarker Cancer
Testing
Live Event: Wednesday, October 9, 2024 |
12:00 - 1:00 PM ET
P.A.C.E.®
credit available until April 9, 2025 | Florida Laboratory Credit
available |
|
Doing More with Smaller Tissue Samples
Traditional next-generation sequencing (NGS) methods, such as hybrid
capture, often require large tissue samples, posing challenges in
clinical scenarios, particularly oncology, where obtaining sufficient
material can be difficult. These limitations can lead to diagnostic
delays and suboptimal treatment decisions that adversely affect patients
and increase costs for healthcare institutions.
In this webinar, explore the advantages of amplicon-based semiconductor
sequencing, a technology that allows for the successful sequencing of
smaller tissue samples. Learn how this approach can overcome the
constraints of traditional methods, improve diagnostic accuracy,
expedite treatment decisions, and enhance overall care. Gain insights
into the practical implementation of amplicon-based semiconductor
sequencing and discover how it can streamline clinical workflows and
deliver better patient outcomes.
This webinar will:
•
Examine the constraints of traditional
sequencing techniques such as hybrid capture
•
Clarify the mechanisms and advantages of
amplicon-based semiconductor sequencing, including its principles,
methodologies, and more
•
Evaluate the practical applications of
amplicon-based semiconductor sequencing in clinical settings and its
impact on clinical and research outcomes
•
Manage the integration of amplicon-based semiconductor sequencing into
existing clinical workflows and research protocols

|
Presenter:
Allison M. Cushman-Vokoun, MD, PhD, FCAP
Director of the Division of Diagnostic Molecular Pathology
and Human Genetics and Medical Director of the Molecular
Diagnostics and Personalized Medicine Laboratory at the
University of Nebraska Medical Center

As a professor at the University of Nebraska Medical Center,
Dr. Cushman-Vokoun oversees molecular biomarker test
development in molecular oncology, with expertise in
next-generation sequencing in solid tumor and hematopoietic
malignancies. She serves as an expert on many national
pathology society committees and is highly involved in
molecular pathology education at the local and national
levels. |
The Impact of Updated Guidelines and Self-collection on Cervical
Cancer Screening
Live Event: Thursday, September 26, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until March 26, 2025 | Florida Laboratory Credit
available |
|
Cervical cancer is the 4th most common cancer among women globally and
95% of cases are due to an HPV infection. Most molecular FDA-cleared HPV
tests report a small number of individual genotypes, with the majority
of them combined into a single pooled result which can impact patient
care and clinical decision making. Additionally, socio-economic and
societal barriers exist that lead to disparities in HPV testing leading
to large numbers of under or unscreened populations and a
disproportionate impact of cervical cancer on these communities.
This webinar will discuss how HPV genotypes in the population have
changed since the introduction of the HPV vaccines as well as how to
adapt to this new paradigm. We will delve into the latest advancements
in HPV testing and ASCCP guideline updates for cervical cancer screening
and explore how HPV extended genotyping can be used to optimize patient
risk stratification and enable HPV persistence tracking. We will also
discuss the value of self-collection in a healthcare setting as a less
invasive testing option to help improve access to cervical cancer
screening. We will examine how these recent advancements are reshaping
screening and management strategies to bring value to clinical
decision-making and patient care.
This webinar will:
•
Describe the changing prevalence of HPV high-risk genotypes due to
vaccination
•
Identify recent changes in ASCCP Guidelines
•
Examine the importance of extended genotyping for patient risk
stratification and management
•
Discuss the impact of FDA-approved HPV tests with self-collection in a
healthcare setting

|
Presenter:
Danielle Clement, M.Ed, MSN, WHNP-BC, AGNP-C
Women’s Health Clinical Manager, BD

Danielle Clement is a Women’s Health Clinical Manager for BD
and a double board-certified women’s health and adult
gerontology nurse practitioner. She holds a Bachelor’s and
Master’s degree in nursing from Duke University, a
certificate in Reproductive Endocrinology and Infertility
from the American Society for Reproductive Medicine (ASRM),
a colposcopy certification from the American Society of
Colposcopy and Cervical Pathology (ASCCP) and is
credentialed as an HIV Specialist with the American Academy
of HIV Medicine (AAHIVM). |
Antigen Testing: How Rapid Results Improve Patient Outcomes
Live Event: Thursday, September 12, 2024 |
12:00 - 1:00 PM ET
P.A.C.E.®
credit available until March 12, 2025 | Florida Laboratory Credit
available |
|
In this webinar, Dr. Young will discuss the critical role(s) and value
of rapid antigen testing at the point-of-care. More specifically, Dr.
Young will explain the relevance of rapid results to better guide
treatment and management decisions in urgent care and other outpatient
clinical settings. He will also discuss lessons learned from last year's
respiratory season and highlight specific steps that healthcare
providers can be taking now to better prepare themselves for the
2024-2025 respiratory season.
This webinar will:
•
Examine the differences between and benefits
of molecular and antigen testing
•
Identify the benefit of Combination Rapid
Antigen Tests during respiratory season
•
Discuss the reasons why testing is so critical at the point of care

|
Presenter:
Stephen Young, PhD D(ABMM)
Medical Director
TriCore Research Institute’s Research and Clinical Trials
Department

Dr. Stephen Young is a Medical Director for TriCore Research
Institute’s Research and Clinical Trials Department. He is
currently the Principal Investigator on 40 FDA clinical
trials, primarily for SARS-CoV-2 EUA detection assays.
Although most of the SARS-CoV-2 trials are still EUA, recent
trials are switching to multiplex respiratory virus
detection.
|
Using Clinical Breakpoints to Improve Antimicrobial Resistance
Detection
Live Event: Wednesday, August 28, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until February 28, 2025 | Florida Laboratory Credit
available |
|
Antimicrobial resistance (AMR) is an urgent global health threat.
Antimicrobial resistance is detected by clinical laboratories that
perform antimicrobial susceptibility tests (AST) against bacteria
isolated from clinical cultures. AST results are interpreted using
clinical breakpoints, which are updated periodically by standards
development organizations and the U.S. Food and Drug Administration
(FDA). Breakpoint changes can benefit patients and public health only if
adopted in a timely manner by diagnostic companies that develop and
market AST products and/or clinical laboratories that perform AST.
Currently, the United States (U.S.) regulatory framework does not compel
laboratories or diagnostic companies to keep up to date with evolving
AST breakpoints. This results in serious patient safety concerns and
hampers the ability to track and contain the worldwide threat of
antimicrobial resistance.
This webinar is an encore presentation of a prior highly regarded
session. It will review results from the recent Open Forum
Infectious Diseases publication Raising the Bar: Improving
Antimicrobial Resistance Detection by Clinical Laboraotires by Ensuring
Use of Current Breakpoints. The new College of American
Pathologists (CAP) requirements to ensure breakpoint adherence will be
discussed and practical examples to address these new requirements will
be provided. By updating clinical breakpoints, we can ensure proper
patient safety and help detect antimicrobial resistance to contain the
threat.
This webinar will:
•
Define the ongoing pandemic of antimicrobial
resistance
•
Discuss how we can address the ongoing
pandemic in the Clinical Microbiology Laboratory
•
Demonstrate the need to apply updated
clinical breakpoints to interpret antimicrobial susceptibility testing
results
•
Review practical examples on how to update clinical breakpoints to
interpret antimicrobial susceptibility testing results for patient care

|
Presenter:
Patricia (Trish) J. Simner, PhD, D(ABMM)
Associate Professor of Pathology
Director of Bacteriology and Infectious Disease Sequencing
Laboratories
Johns Hopkins University School of Medicine

Dr. Trish Simner is an Associate Professor of Pathology and
Infectious Diseases at the Johns Hopkins University School
of Medicine and the Director of the Medical Bacteriology and
Infectious Disease Sequencing Laboratories at the Johns
Hopkins Hospital. She completed her PhD at the University of
Manitoba in Manitoba, Canada and a two year Clinical
Microbiology Fellowship at the Mayo Clinic. She is widely
regarded internationally as an expert in the field of
mechanisms of antimicrobial resistance and antimicrobial
susceptibility testing. |
Pharmacogenetics in Practice: Case Studies & Considerations for
Effective Implementation
Live Event: Thursday, August 22, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until February 22, 2025 | Florida Laboratory Credit
available |
|
Pharmacogenetics (PGx) has potential to achieve the practice of
precision medicine, but challenges exist. Issues such as lack of
provider/patient education, absence of clinical decision support, and
unclear reimbursement are significant barriers to the implementation of
PGx in a scalable manner. In this webinar, several case studies will be
examined that highlight the process of evaluating PGx reports and how
they can be used in a clinical context. Furthermore, important
considerations for providers for the effective implementation and
scaling of PGx in the clinic will be discussed.
This webinar will:
•
Describe how PGx reports can be reviewed
•
Discuss the limitations of PGx reports and how they can be used in a
clinical context
•
Identify important factors for effective implementation of PGx in a
clinical setting
•
Examine the existing challenges to scale PGx as a precision medicine
tool and ways to address these challenges
 |
Presenter:
Jeremy Stuart, Ph.D, MPH (NRCC)
Chief Scientific Officer and Laboratory Director
Precision Genetics
Greenville, SC

Dr. Jeremy Stuart has extensive experience in the life
science industry. He specializes in commercial operations,
technology development and transfer, manufacturing design,
start up and analytical validation of laboratory developed
tests (LDTs). He currently serves as the Chief Scientific
Officer for Precision Genetics and serves as their
Laboratory Director. |
Using Molecular GI Testing to Improve Laboratory Efficiency and
Patient Management
Live Event: Wednesday, July 17, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until January 17, 2025 | Florida Laboratory Credit
available |
|
Gastrointestinal infections challenge the healthcare system, creating a
major burden for the hospital, both operationally and financially.
Traditional diagnostic methods such as culture, microscopy and
immunoassays come with limitations that potentially impact laboratory
operations, clinical decision-making and patient outcomes.
The impact of implementing molecular testing methods for GI pathogens
can offer multiple benefits compared to traditional methods. These could
include differences in turnaround time, positivity rates, sensitivity,
laboratorian hands on time, patient length of stay, and antimicrobial
usage.
In this webinar, you will hear from an experienced clinical
microbiologist on their selection criteria for molecular panels for GI
testing, the impact it has had on their laboratory and patients, and the
role diagnostic stewardship plays in their laboratory testing practices.
This webinar will:
•
Discuss the impact of targeted enteric panels on laboratory workflow and patient management
•
Review considerations for diagnostic
stewardship in molecular GI testing
•
Identify the factors that lead to selection of different molecular
panels

|
Presenter:
Jennifer Dien Bard PhD, D(ABMM), FIDSA, FAAM
Professor of Pathology, Keck School of Medicine, University
of Southern California
Director, Clinical Microbiology and Virology Laboratories,
Department of Pathology and Laboratory Medicine
Children’s Hospital Los Angeles

Dr. Dien Bard is a Professor of Pathology with Clinical
Scholar designation in the Department of Pathology, Keck
School of Medicine, University of Southern California. She
is the Director of the Clinical Microbiology and Virology
Laboratories in the Department of Pathology and Laboratory
Medicine at Children’s Hospital Los Angeles. |
The Impact of Antimicrobial Stewardship and Accurate
Susceptibility Results on Patients with Sepsis
Live Event: Wednesday, June 26, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until December 26, 2024 | Florida Laboratory Credit
available |
|
Sepsis is a leading cause of morbidity, mortality resulting in more than
250,000 deaths in the US annually and is a major driver impacting health
system costs. Current rapid diagnostics do not adapt well to providing
an accurate diagnosis and prognosis of acute infections and sepsis.
Clinical decisions including timing and dosage of therapy and
level-of-care decisions rely on understanding etiology and implications
of a clinical presentation.
Early treatment with appropriate antibiotics has been shown to reduce
morbidity and mortality in cases of bacterial sepsis. However, an
estimated 20% of hospitalized patients treated with parenteral
antibiotics experiences an adverse drug event and more than 2 million
people experience antibiotic-resistant infections each year.
Indiscriminate and prolonged use of antibiotics can lead to
antimicrobial resistance. Adherence to effective stewardship practices
and rapid, accurate assessment and treatment of patients with acute
infections and sepsis can significantly impact the probability of
survival.
Effective diagnostic solutions could improve management of patients with
suspected acute infections and sepsis, thereby lessening the overall
burden of these conditions on patients and the healthcare system. Access
to newer antibiotics and diagnostics that can provide accurate MICs for
effective treatment of critical patients can reduce length of stay,
adverse effects and overall costs to the system while significantly
improving patient outcomes.
This webinar will:
•
Evaluate testing options for the rapid
identification of sepsis and antibiotic-resistant infections
•
Demonstrate the need for new therapeutics to
accompany accurate diagnostics to reduce cost and risk
•
Demonstrate the impact of effective therapy
on survival rates of patients with acute infections and sepsis
•
Impact of effective stewardship practices on mortality and how accurate
laboratory data can guide appropriate decision making

|
Presenter:
Nathan Ledeboer, PhD
Professor of Pathology & Laboratory Medicine
Chief, Clinical Pathology, Medical College of Wisconsin &
Associate Chief Medical Officer for Laboratory Services
Froedtert Health

Dr. Ledeboer is the director of medical and technical
activities for laboratory services at Froedtert and the
Medical College of Wisconsin. In this role, he oversees
development and implementation of new assays, sign out of
all testing performed in these laboratories, and consults
with physician colleagues regarding test results and
selection. |
The Anti-Xa Assay: Therapeutic Monitoring of Heparin
Live Event: Thursday, June 20, 2024 |
12:00 - 1:00 PM ET
P.A.C.E.®
credit available until December 20, 2024 | Florida Laboratory Credit
available |
|
Heparin is an anticoagulant used to prevent and treat blood clots in
at-risk patients. Heparin exists in two forms- unfractionated heparin
(UFH) and low-molecular-weight heparin (LMWH)- both of which
considerably accelerate the inactivation of coagulation factor Xa by
antithrombin. Heparin assays are often referred to as anti-Xa assays for
this reason. The anticoagulant activity of UFH is somewhat
unpredictable. Conversely, LMWH anticoagulant activity is more
consistent and predictable.
Traditional monitoring of UFH has been done using the APPT assay.
However, the assay is fought with pre- and post-analytical and
analytical variations. Alternative methods may need to be used to
monitor the variable and unpredictable nature of UFH. Therefore, close
laboratory monitoring to guide dosing adjustments is often needed. This
presentation is designed for laboratorians who are interested in
learning more about heparin monitoring and exploring utilization of
anti-Xa assays in their institutions.
This webinar will:
•
Describe the anticoagulant effects of
heparin
•
Explain the methods used to determine
heparin concentration
•
Determine the limitations of the anti-Xa
assay
•
Formulate an approach for conversion to utilizing anti-Xa assay for
anticoagulant monitoring

|
Presenter:
Dr. John V. Mitsios, PhD
Medical and Scientific Affairs
Medical Sciences Partner
Siemens Healthcare Diagnostics

Dr. Mitsios graduated from the University of Ioannina,
Greece with a PhD in Chemistry. Upon completion of his
doctoral thesis, he then went on to complete a post-doctoral
fellowship at the University of California, San Diego. Dr.
Mitsios then transitioned to the world of Clinical Chemistry
and completed a fellowship at Washington University in St.
Louis, MO. |
Sample Preparation for Clinical LC-MS Assays
Live Event: Thursday, June 13, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until December 13, 2024 | Florida Laboratory Credit
available |
|
Biological samples used for clinical testing must be appropriately
prepared to reduce complexity and potential system contaminants prior to
analysis by liquid chromatography-mass spectrometry (LC-MS). Inadequate
sample preparation will adversely affect clinical testing by reducing
the accuracy and precision of results, as well as increasing the
instrument downtime and need for maintenance and repair. This has
implications for both the quality of patient care and also the financial
health of the institution where testing takes place.
This webinar will provide a discussion of appropriate sample preparation
techniques for clinical LC-MS methods based on the clinical application
and sample type. The session will encompass various sample preparation
approaches used for LC-MS (liquid chromatography coupled to mass
spectrometry) assays. It will also highlight the importance of sample
processing in the clinical laboratory environment and illustrate the
“fit for purpose” application of processing techniques in clinical mass
spectrometry.
This webinar will:
•
Describe various pain points and challenges
in clinical LC-MS
•
Discuss the impact of various specimen
preparation approaches on LC-MS assay performance
•
Implement a fit-for-purpose approach to
selection of a specimen preparation approach in their laboratory
practice
•
Describe alternative specimen and microsample types and the limitations
that must be considered for specimen preparation

|
Presenter:
William Clarke, PhD, MBA, DABCC
Professor of Pathology
Deputy Director, Quality and Regulatory Affairs; Pathology
Johns Hopkins University School of Medicine

Dr. Clarke received his Ph.D. in Analytical Chemistry from
the University of Nebraska in Lincoln in 2000, followed by a
post-doctoral fellowship in Clinical Chemistry at the Johns
Hopkins School of Medicine, ending in 2002. In addition, he
received an MBA focused on medical services management from
the Carey School of Business at Johns Hopkins in 2007.
|
Importance of Microscope Slides and Coverglass in the Laboratory
Live Event: Thursday, May 30, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until November 30, 2024 | Florida Laboratory Credit
available |
|
Microscope slides and coverglass are used in many parts of the lab while
knowledge of how these items are made and the technical properties they
have is limited. By not understanding the properties of the key
component of many tests in the lab, registrants may not know what’s
causing some issues during their testing. Due to the attributes of
different types of slides, it can cause different adherence of samples
to the slide and influence the turnaround time and possibly the results
of patient tests.
During the webinar, registrants will learn how the slides are
manufactured, what types of adhesion chemistry are available in the
market and how the various slide types can help them improve their
workflow and results for patients.
This webinar will:
•
Explain glass manufacturing process
•
Identify what makes adhesion properties on
slides
•
Assess utility of different types of slides
•
Discuss importance of coverglass specifications
 |
Presenter:
Rachel Rosenblum
Sr. Regional Marketing Manager, Epredia

Rachel has over 13 years of experience in the biotech
industry. She is a Marketing manager for Epredia with
portfolios that include microscope slides and coverglass,
slide and cassette labeling equipment along with other
histology consumables and instrumentation. She also has
expertise in precision medicine, chemiluminescence, data
management software and cybersecurity for instrument
platforms.
|
Advancing Urgent Care POC to Combat the Ongoing STI Epidemic
Live Event: Tuesday, May 28, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until November 28, 2024 | Florida Laboratory Credit
available |
|
Most Chlamydia trachomatis/Neisseria gonorrhoeae (CT/NG) testing in
urgent care involves send out tests that can take 2-7 days for results.
This forces urgent care providers to make treatment decisions without
the benefit of test results.
Rapid POC CT/NG testing allows providers to make informed decisions
about when to treat with antibiotics and when NOT to treat. It will also
provide greater opportunity for patient education and partner expedited
therapy. National screening rates under CDC guidelines are poor (<50%),
and rapid POC CT/NG testing has potential to effect an improvement in
screening.
This webinar will examine key challenges with STI testing today in
Urgent care including patients lost to follow-up, implications of
overtreatment/undertreatment of STI, review applicable CDC STI Treatment
& Screening Guidelines, discuss sexual health education strategies for
STIs in young people, examine the importance of timely STI diagnosis and
appropriate treatment, discuss definitive/directed antibiotic therapy vs
empiric/presumptive treatment, and evaluate the implications of today’s
STI testing to Antibiotic Stewardship.
This webinar will:
•
Examine key challenges with STI testing
today in Urgent care including patients lost to follow-up, implications
of overtreatment/undertreatment of STI
•
Review applicable CDC STI Treatment &
Screening Guidelines
•
Discuss sexual health education strategies
for STIs in young people
•
Examine the importance of timely STI
diagnosis and appropriate treatment
•
Discuss definitive/directed antibiotic therapy vs empiric/presumptive
treatment
•
Evaluate the implications of today’s STI testing to Antibiotic
Stewardship

|
Presenter:
Glenn Harnett, MD
CEO No Resistance Consulting Group, LLC

Dr. Harnett has spent over 20 years as a "boots on the
ground" clinician, spending 10 years as an emergency
physician before establishing himself as a nationally
respected physician and key opinion leader in urgent care.
In addition, he has been an active author and researcher -
designing trials, writing trial protocols, and acting as a
principal investigator for numerous clinical trials
conducted in the urgent care setting. After spending 5 years
as the Chief Medical Officer for American Family Care as
they grew from 17 to 185 clinics, he founded No Resistance
Consulting Group in 2016 which focuses on clinical trial
site management and recruitment for a growing network of
high volume, geographically diverse, urgent care and
multi-specialty sites. |
Differentiation of HSV & VZV Lesions Using Multiplex Molecular
Testing
Live Event: Tuesday, May 7, 2024 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until November 7, 2024 | Florida Laboratory Credit
available |
|
Herpes viruses, specifically herpes simplex virus (HSV) and varicella
zoster virus (VZV), are some of the most common causes of primary and
latent oral, genital, and cutaneous lesions. It is often difficult to
visually differentiate HSV-1, HSV-2, VZV, and multiple other
lesion-causing etiologies. While primary antiviral treatment of HSV and
VZV are often the same, the need to treat, duration of treatment, and
recurrence prevention differ, as does rate of recurrence,
transmissibility, and long-term complications. Therefore, it is
imperative that suspected lesions be diagnosed accurately.
Diagnostic challenges indicate a role for rapid molecular multiplex
testing that can assess multiple lesion-causing pathogens, ideally while
a patient is still present for education and treatment. This webinar
will discuss the prevalence of herpes virus-related lesions, discuss the
importance of viral differentiation, evaluate diagnostic challenges, and
provide information on utilizing rapid near-patient molecular multiplex
testing to improve lesion diagnosis.
This webinar will:
•
Review the prevalence of herpes
virus-related lesions
•
Discuss the clinical importance of
differentiating HSV-1, HSV-2, & VZV
•
Determine diagnostic challenges associated
with herpes virus lesions and how a molecular multiplex assay can
improve diagnostic accuracy
•
Identify how rapid near-patient molecular testing can improve workflow
and patient outcome

|
Presenter:
Preeti Pancholi, PhD, D(ABMM)
Director, Clinical Microbiology
Professor, Clinical Pathology
The Ohio State University
College of Medicine
Wexner Medical Center
Columbus, OH

Preeti Pancholi, PhD is a Professor and Director of the
Clinical Microbiology Laboratory at The Ohio State
University Wexner Medical Center, Columbus, OH. In this
role, she is responsible for the daily management of
clinical microbiology laboratory offering infectious
diseases diagnostic testing. She is board certified and has
over 20 years of experience in clinical microbiology. |
Microbiology Results for Critical Patients: A 2023 Perspective
Live Event: Wednesday, December 13, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until June 13, 2024 | Florida Laboratory Credit
available |
|
The role of the microbiology laboratory and the choice of antimicrobial
susceptibility testing (AST) method is crucial to determining the
appropriate treatment for severe infections in critically ill patients.
Delayed or inaccurate results, especially for patients with multi-drug
resistant infections, can lead to less effective treatment and potential
mortality.
Accurate minimum inhibitory concentration (MIC) data can reduce
turn-around times and favorably impact therapeutic decisions. The use of
new generation therapeutics like sulbactam/durlobactam and MIC results
for determining optimal treatment are critical in the face of growing
antibiotic resistance. The availability of accurate broth
microdilution-based MICs for new antibiotics can help improve patient
outcomes and reduce the lengths-of-stay, therapeutic dosages and
duration, adverse reactions, and costs.
Actions taken by the antimicrobial stewardship team to enforce the
judicious use of antimicrobials are most effective when supported by
timely diagnostic information from and collaboration with microbiology
laboratory personnel. Effective collaborations among microbiologists,
clinicians, the antimicrobial stewardship team, and policy makers can
help improve patient care and meet the challenges of increased
antibiotic resistance in a post-Covid world.
This webinar will:
•
Review the challenges of treating and
managing critically ill patients
•
Describe how MIC results for new generation
therapeutics are used to manage patient care
•
Summarize how effective diagnostic and
antimicrobial stewardship can help combat resistance
•
Explain the importance of MIC results and breakpoints
|
Presenter:
James A. McKinnell, MD
Associate Professor of Medicine
David Geffen School of Medicine, UCLA
Division of Infectious Disease, LA-Biomed at Harbor UCLA
Medical Center
James A. McKinnell, M.D. is an Associate Professor of
Medicine at the David Geffen School of Medicine at the
University of California, Los Angeles. He is also a member
of the Infectious Disease Clinical Outcome Research Unit
(ID-CORE) and the Los Angeles Biomedical Research Institute
at Harbor-UCLA. Dr. McKinnell is a nationally-recognized
infectious disease specialist with specific research
interests related to the clinical management and prevention
of healthcare-associated infections.
|
Revitalizing Diabetes Care in Primary Care: Improving Clinical
Inertia for Diabetes Management
Live Event: Tuesday, November 21, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until May 21, 2024 | Florida Laboratory Credit
available |
|
Join our upcoming webinar, “Revolutionizing Diabetes Management,” to
tackle the growing diabetes prevalence. We’ll address clinical inertia,
which hinders optimal care, and explore ways to democratize healthcare
for better patient outcomes. Discover cutting-edge technologies, patient
empowerment, and inclusive practices that can transform diabetes
management in the primary care setting reducing the burden on
individuals and society. Don’t miss this opportunity to be a part of the
fight against diabetes.
This webinar will:
•
Review the current situation for managing
people living with diabetes in the primary care setting today
•
Discuss the impact of diabetes management on
patient outcomes and quality of care
•
Examine the measures that treating
healthcare providers can implement to improve their diabetes management
program by addressing clinic inertia and democratizing healthcare
•
Identify the effects of empowering patients
and intervening earlier
•
Analyze available diabetes management methods to reduce the economic
burden on people and healthcare systems

|
Presenter:
Aaron King, MD
Family Medicine and Diabetes Specialist
MedFirst Primary Care
San Antonio, TX

Dr. Aaron King is a Family Medicine and Diabetes Specialist
at MedFirst Primary Care, a Baptist Medical Center
affiliate. Dr. King graduated from the University of Texas
with a B.S. in Microbiology and top of his class at Texas
A&M Medical School, while on a scholarship with the United
States Navy through the HPSP program. After his USN
commission, Dr. King became ABFM certified in Family
Medicine after his residency at Navy Hospital Pensacola. |
Improved Lab Efficiency by Automating Urine Plate Reading
Live Event: Wednesday, November 15, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until May 15, 2024 | Florida Laboratory Credit
available |
|
Chronic staffing shortages along with increased workload have led many
microbiology laboratories, to consider automation. While this seems
like a practical approach, there are many important considerations in
making such a decision including cost, space, accuracy, ease of use and
compatibility with already established lean workflows.
This webinar will discuss how advances in artificial
intelligence-enabled laboratory automation can help labs automatically
read and interpret microbial cultures. By using proprietary algorithms
for enumeration and classification of growth the system can improve
accuracy and workflow efficiency.
The webinar will also illustrate the impact of AI based automation on
laboratory time, describe how automation categorizes the difference
between significant and non-significant growth from urine cultures, and
discuss how standalone automation can be installed and integrated into a
labs lean workflow.
This webinar will:
•
Examine the impact of AI based automation on
laboratory time
•
Describe how automation categorizes the
difference between significant and non-significant growth from urine
cultures
•
Discuss how standalone automation can be
installed and integrated into a labs lean workflow
|
Presenter:
Mary George, PhD, D (ABMM)
Director Microbiology Lab, Department of Pathology and
Laboratory Medicine, Albany Med Health System
Assistant Professor, Albany Medical College

Dr. Mary George has over 40 years of clinical microbiology
laboratory experience as both a Medical Laboratory Scientist
and laboratory Director. Currently she is Director of the
Microbiology Laboratory at Albany Medical Center in Albany,
NY. She obtained her Ph.D. in Medical Microbiology from Wake
Forest University School of Medicine and completed
postdoctoral training in Medical and Public Health
Laboratory Microbiology at the University of North Carolina
Medical Center. |
Acute Pharyngitis: Advances in Pathogen Identification &
Diagnosis
Live Event: Wednesday, October 25, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 25, 2024 | Florida Laboratory Credit
available |
|
Acute pharyngitis is one of the most common reasons for primary care
visits and is the most common diagnosis linked to antibiotic use in
school-aged children. Due to extended turnaround times associated with
culture and low sensitivity of rapid antigen detection testing (RADT),
many clinicians empirically prescribe antibiotics to prevent severe
sequelae associated with Group A Streptococcus (GAS).
While GAS accounts for a substantial number of pharyngitis infections,
recent studies suggest that non-GAS bacteria including Groups C and G
Streptococcus may also lead to pharyngitis and be as prevalent as GAS
within certain populations. RADTs often lack sensitivity and do not test
for non-GAS bacteria or viruses, leaving labs to perform time-consuming
culture to determine causative etiologies for pharyngitis. This webinar
will address the complexities of acute pharyngitis diagnosis and
summarize emerging clinical data on non-GAS pathogens, current testing
methods, and the potential role of point-of-care molecular and multiplex
testing for pharyngitis pathogens.
This webinar will:
•
Discuss the types of pathogens that cause
pharyngitis
•
Review emerging pathogens that may mimic
group A Streptococcus pharyngitis
•
Evaluate the attributes of molecular
multiplex platforms for pharyngitis
•
Identify the benefits of point-of-care, patient-centered testing with
regard to diagnosis, treatment, and workflow
 |
Presenter:
Bobby L. Boyanton Jr, MD
Professor of Pathology
University of Arkansas for Medical Sciences
Pathologist-in-Chief and Section Medical Director,
Molecular Pathology
Arkansas Children’s Hospital

Bobby L. Boyanton Jr., M.D., is a Professor of Pathology at
the University of Arkansas for Medical Sciences, and
Pathologist-in-Chief and Section Medical Director of
Molecular Pathology at Arkansas Children’s Hospital. He
oversees all aspects of the clinical laboratories and the
point-of-care testing program for the hospital and
affiliated clinics. His passion lies in the molecular-based
diagnosis of infectious diseases within both the laboratory
and point-of-care settings.
|
Common Chronic Liver Disease: Causes & Laboratory Testing Solutions
Live Event: Tuesday, October 24, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 24, 2024 | Florida Laboratory Credit
available |
|
In 2020, chronic liver disease was the 12th leading cause of death in
the United States. Chronic liver disease involves the progressive
destruction and regeneration of liver tissue that leads to fibrosis and
cirrhosis. Cirrhosis and chronic liver failure are leading causes of
morbidity and mortality, with most cases attributed to excessive alcohol
consumption, viral hepatitis B or C, or nonalcoholic fatty liver
disease. From the results of multiple studies, these four conditions
account for approximately 80% of all chronic liver disease.
This presentation focuses on the epidemiology, clinical aspects, signs
and symptoms, and diagnosis of these four common causes of chronic liver
disease. It also considers the value of direct assessment for
identifying at-risk patients. Finally, it examines the utility of the
Enhanced Liver Fibrosis (ELF) Score in assessing the likelihood of
progression to cirrhosis and liver-related clinical events in patients
with advanced fibrosis.
This webinar will:
•
Describe four main causes of chronic
liver disease
•
Discuss major risk factors for developing
chronic liver disease
•
Explain associated clinical and laboratory findings
•
Summarize testing options to assist in the
differential diagnosis of chronic liver disease

|
Presenter:
Jim Aguanno, PhD
Senior Clinical and Scientific Consultant
Siemens Healthineers

Dr. James Aguanno received a Ph.D. in Biochemistry from
Memphis State University. Following his Ph.D., he did two
post-doctoral fellowships one at the University of
Pittsburgh School of Medicine in Biochemistry and a second
fellowship in Laboratory Medicine at Washington University
School of Medicine and Barnes Hospital in St. Louis,
Missouri. |
Automated Susceptibility Testing to Optimize Patient Outcomes
Live Event: Thursday, October 5, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 5, 2024 | Florida Laboratory Credit
available |
|
The focus on antibiotic stewardship is increasing and will be mandated,
with the focus on providing optimal care, and reducing unnecessary
antibiotic exposure risk for developing MDR infections. The link between
the stewardship team and the microbiology laboratory is critical for
success. Obtaining timely and accurate organism identification and
susceptibility data is essential in conducting daily antibiotic
stewardship activities. Identifying key priorities for success has a
significant influence over the criteria used when selecting automated
systems for the lab. The data generated from these systems reflexes to
real-time review and intervention by the Stewardship Team.
Multidisciplinary collaboration is essential in optimizing patient
outcomes. This webinar will describe the impact of effective stewardship
practices on mortality and how collaboration between the microbiology
lab and stewardship team can improve metrics, review the impact of
effective stewardship practices in cases of sepsis and septic shock, and
demonstrate the need for new therapeutics to accompany accurate
diagnostics.
This webinar will:
•
Describe the impact of effective stewardship
practices on mortality and how collaboration between the microbiology
lab and stewardship team can improve metrics
•
Review the impact of effective stewardship
practices in cases of sepsis and septic shock
•
Demonstrate the need for new therapeutics to accompany accurate
diagnostics
|
Presenter:
Jerod Nagel, PharmD, BCIDP
Clinical Pharmacist Specialist in Infectious Diseases
Residency Program Director: PGY2 Infectious Diseases
Adjunct Clinical Assistant Professor in Pharmacy

Dr. Jerod Nagel is the pharmacy team lead for the Infectious
Diseases & Antimicrobial Stewardship Program at the
University of Michigan Health Systems. Currently the program
has 3 specific daily patient care responsibilities:
drug-based stewardship, outcomes-based stewardship and ID
consult. His team is heavily involved in QI initiatives
linked to reimbursement and joint commission standards,
which require collaborations with a numerous groups across
the health care system.
|
Decalcification for Routine, Advanced, and Molecular Analysis
Live Event: Wednesday, September 27, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until March 27, 2024 | Florida Laboratory Credit
available |
|
Quality sample preparation is fundamental to the analytical process.
Various methods have been employed for decalcification including use of
acids, chemical agents, and electric and ultrasonic means. The purpose
of decalcification is to remove calcium salts from mineralized tissue,
resulting in preservation of organic components so that paraffin
sections can be prepared for histological assessment. It is important to
choose a proper decalcification method and timing for every specimen
being handled. Specimens that are subjected to molecular testing might
require special attention and procedures.
This webinar will:
•
Describe the nature of calcified tissues and
the need for decalcification
•
Identify the different decalcification
methods and evaluate their advantages and limitations
•
Examine the process of choosing an optimal
decalcification method
•
Discuss the effects of decalcification
protocols on IHC and molecular assays

|
Presenter:
Andrew Lisowski, MS, HTL(ASCP)
Senior Technical Content Global Marketing Manager, Epredia

Andrew Lisowski has almost 30 years of experience in
histology and histotechnology. He attended veterinary school
and earned his master’s degree in molecular biology. He
worked in histology, IHC and ISH labs, cell culture lab,
performed in-vitro and in-vivo toxicology assays and was a
member of a necropsy team. Andrew worked for pharmaceutical
companies, medical schools and founded his own molecular and
histology firms. Currently, he is the Senior Technical
Content Manager at Epredia providing global technical
content.
|
Fighting the Rise of STI Rates with Rapid Testing and Early
Detection
Live Event: Wednesday, August 23, 2023 |
2:00 - 3:00 PM ET
P.A.C.E.®
credit available until February 23, 2024 | Florida Laboratory Credit
available |
|
With the increasing rates of Sexually Transmitted Infections (STIs)
across the country, early diagnosis of an infection is a critical and
often challenging aspect in today’s healthcare system. HIV and syphilis
are both serious infections that can have devastating consequences on
their own, including co-infection, transmission to others, and increased
risk of acquiring other STIs1.
Identifying patients with these infections accurately and rapidly is
integral in preventing transmission and connecting patients to care, but
it can be a sensitive process for the patients and daunting for clinical
staff.
This program will cover current HIV and syphilis statistics, risk
factors, testing guidelines and recommendations, and newly approved
technology to aid in the rapid diagnosis of both conditions and
subsequent care for all patient populations in need.
Reference:
1https://hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-and-sexually-transmitted-diseases-stds
This webinar will:
•
Review the most current HIV & syphilis US
surveillance data
•
Explain the current testing guidelines for
HIV & syphilis
•
Describe the importance of dual testing for
HIV and syphilis & the benefits of rapid testing
•
Summarize HIV & syphilis testing methods & algorithms

|
Presenter:
Matthew M. Hamill, M.B.Ch.B.
Johns Hopkins Bayview Medical Center, Division of
Infectious Diseases
Dr. Matthew Hamill is interested in all aspects of Sexually
Transmitted Infections (STI) and HIV including prevention,
treatment, and retention in care. His research focuses on
rapid, Point-of-Care diagnostics for STI in low-income
settings. He provides patient-focused treatment for those
with, or at risk of, STI and HIV. Dr. Hamill is affiliated
with Johns Hopkins School of Medicine and the Bloomberg
School of Public Health. |
How to Start an NGS Lab for Reproductive Health Research
Live Event: Wednesday, August 16, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until February 16, 2024 | Florida Laboratory Credit
available |
|
The field of reproductive health has grown significantly, and the
technology used for genetic testing has matched this growth. In the past
15 years, we’ve seen techniques such as fluorescence in situ
hybridization (FISH), array-based methods, and a move to the current
standard of next-generation sequencing (NGS) take hold as routine
methods for preimplantation genetic testing and carrier screening
research. While the move to faster and more efficient methods has made
these applications more accessible, it has also introduced a new layer
of complexity to the lab.
The advantages of gaining more information from a higher resolution
platform or the ability to perform multiple applications on a single
platform may be worth the hurdle of bringing on a new methodology. While
NGS tends to have an easier workflow, there are other considerations for
those unfamiliar with molecular testing. This webinar will outline what
is required to start a new NGS lab for reproductive health research and
address the analytical validation requirements for high-complexity labs.
This webinar will:
•
Identify the equipment needed for a new
molecular lab
•
Assess space requirements for
instrumentation, workbenches, and storage spaces
•
Evaluate personnel requirements for CLIA and
CAP and associated credentials
•
Review analytical validation steps and consulting services for research
workflows
|
Presenters:
 Alain
Rico Alain
Rico
Senior Manager Global Market Development,
Reproductive Health, Thermo Fisher Scientific, France
 Matt
Osentoski Matt
Osentoski
Sr Manager, Project Management, Global NGS
Analytical Validation Services, Thermo Fisher Scientific,
U.S. |
The Value of Rapid Antigen Testing
Live Event: Wednesday, July 12, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until January 12, 2024 | Florida Laboratory Credit
available |
|
The SARS-CoV-2, influenza (flu), and respiratory syncytial virus (RSV)
tripledemic of the 2022–2023 U.S. respiratory season posed a challenge
for both patients and the healthcare system. In this webinar, the
presenter will discuss lessons learned and the value of using rapid
antigen testing to detect these viruses.
As we progress toward the next respiratory season, healthcare facilities
across the industry need to prepare to address simultaneous SARS-CoV-2,
flu, and RSV outbreaks once again. By gaining access to low-cost,
easy-to-use rapid antigen tests, clinicians can be better equipped to
differentiate these viral infections so providers can offer more
accurate diagnoses and treatment.
This webinar will:
•
Explain the overall value and differences between molecular and antigen
testing
•
Discuss the respiratory disease state and the recent tripledemic in the
US
•
Describe the benefit of combination rapid antigen testing during
respiratory seasons
 |
Presenter:
Dr. Amesh Adalja, MD

Dr. Amesh Adalja works as an adjunct assistant professor at
Johns Hopkins University, Carnegie Mellon University, and
the University of Pittsburgh. He is also a senior scholar at
the Johns Hopkins Center for Health Security and an
affiliate of the Johns Hopkins Center for Global Health. Dr.
Adalja is board certified in infectious disease, critical
care, emergency, and internal medicine and actively
practices in the Pittsburgh area. His other areas of focus
include emerging infectious diseases, pandemic preparedness,
and biosecurity. |
Ergonomics in the Lab: Increasing Productivity
Live Event: Tuesday, June 20, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until December 20, 2023 | Florida Laboratory Credit
available |
|
Laboratories provide many opportunities for
ergonomic stressors to manifest into injuries or repetitive stress
disorders. Major ergonomic issues in the laboratory setting include
static and/or awkward postures and repetitive motions. Could you
identify these most common hazards in a clinical / diagnostic laboratory
work environment? Compare your laboratory to others from Dan the Lab
Safety Man based on his 30+ years of experience working in, managing,
and leading the lab’s safety programming.
You will want to attend this webinar to learn
about ergonomics in labs that our presenter has experienced, addressed
and shared with safety and laboratory colleagues during his experiences
touring and inspecting clinical laboratories in healthcare. We will
identify the top most frequently seen ergonomic hazards in a healthcare
laboratory and provide cost-effective solutions to avoid these everyday
hazards. Most importantly, the webinar will provide a greater
understanding of how participants can keep the people around them safe
in their healthcare laboratory.
This webinar will:
•
Review basic and intermediate laboratory
safety regulations and applications
•
Examine specific lab ergonomic subjects
•
Identify cost effective solutions to these
everyday hazards
•
Relate laboratory needs to specific lab safety products
|
Presenter:
Dan Scungio, MT(ASCP), SLS, CQA(ASQ)

Daniel J. Scungio has over 30 years of experience as a
certified Medical Technologist. After 10 years of lab
management, he became the Laboratory Safety Officer for a
system of more than 10 hospitals and over 20 laboratories
and draw sites in Virginia and North Carolina. As a
laboratory safety consultant and a safety officer, Dan has
provided on-site education and safety training for labs of
all sizes. He has become an international speaker and
consultant who helps organizations create safety savvy
laboratories.
|
Tissue Processing: Frequently Asked Questions
Live Event: Tuesday, May 16, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until November 16, 2023 | Florida Laboratory Credit
available |
|
Tissue Processing is the most complex and one of the longest steps in
the histology workflow. Since the processing step is overly complex,
mistakes are quite common, and questions arise about possible remedies
and corrective actions. In this webinar, we will answer frequent
questions related to tissue processing. Understanding the science of
processing, consumable interactions will increase tissue quality,
therefore, enabling a faster diagnosis that can be delivered to the
patient, promoting better patient care.
This webinar will:
•
Examine ways to avoid common mistakes
•
Discuss the ways to take corrective action
•
Analyze simple chemical interactions
•
Discuss the reason behind reagent composition
 |
Presenter:
Andrew Lisowski, MS, HTL(ASCP)
Senior Technical Content Global Marketing Manager
Epredia

Andrew Lisowski has almost 30 years of experience in
histology and histotechnology. He attended veterinary school
and earned his master’s degree in molecular biology. He
worked in histology, IHC and ISH labs, cell culture lab,
performed in-vitro and in-vivo toxicology assays and was a
member of a necropsy team. Andrew worked for pharmaceutical
companies, medical schools and founded his own molecular and
histology firms. Currently, he is the Senior Technical
Content Manager at Epredia providing global technical
content.
|
STI Testing – What to Offer & How to Offer It
Live Event: Wednesday, May 10, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until November 10, 2023 | Florida Laboratory Credit
available |
|
The number of cases of sexually transmitted infections (STI) around the
world has been on the rise for years. Given the variability in screening
and testing guidelines for treatable STIs, what should your lab be
offering to clients? The answer, of course, depends on the patient
populations being served.
This webinar will discuss for whom and under what circumstances to test
for Chlamydia trachomatis, Neisseria gonorrhoeae,
Trichomonas vaginalis, and Mycoplasma genitalium. In
addition to decisions about appropriate test menus, we will discuss
acceptable sample types — including non-genital specimens — and sample
collection methods, including remote sample collection. This discussion
will also cover regulatory aspects that impact a lab’s ability to offer
different types and levels of testing.
This webinar will:
•
Explain how to determine whether Mycoplasma genitalium
testing is appropriate for a patient according to CDC guidelines
•
Identify when non-genital STI testing is appropriate
•
Apply regulatory considerations when determining how to proceed
(or why not to proceed) with offering remote sample collection for
testing in your laboratory
|
Presenters:
 Barbara
Van Der Pol, PhD, MPH Barbara
Van Der Pol, PhD, MPH
Professor of Medicine
Division of Infectious Diseases
University of Alabama at Birmingham
 Obiageli
(Oby) Okafor, MD, DrPH Obiageli
(Oby) Okafor, MD, DrPH
Sr. Manager, Product Applications
Global Health Equity
Thermo Fisher Scientific |
Interdisciplinary Teams Are Key to Successful Antimicrobial
Stewardship
Live Event: Wednesday, January 25, 2023 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until July 25, 2023 | Florida Laboratory Credit
available |
|
New drug development has been in decline and antimicrobial resistance
has been steadily on the rise. This dynamic has resulted in the
development of multi-drug resistant microorganisms (MDRO) and challenges
in managing the resulting complicated infections. Antimicrobial
Stewardship Programs have key objectives to promote the appropriate use
of antimicrobials, improve patient outcomes, reduce microbial resistance
and decrease the spread of infections caused by MDROs.
Multi-drug resistance is particularly challenging for institutions to
manage, specifically when transmitted among vulnerable patient
populations. Optimal therapeutic options may be few and limited by
toxicity that can further compromise patient health. Accurate diagnostic
tools that can guide the most appropriate clinical decisions in these
life-threatening infections with is critical.
Microbiology laboratories with access to accurate antimicrobial
susceptibility platforms that include drugs of last resort as well as
novel drugs can lead to more effective and optimal treatment decisions,
reducing cost of stay and improving patient outcomes.
This webinar will:
•
Evaluate testing options for the rapid
identification of resistant infections
•
Demonstrate the need for new therapeutics to
accompany accurate diagnostics
•
Review the impact of COVID on the
development Antimicrobial Resistance
•
Discuss the impact of effective stewardship practices on mortality and
how accurate laboratory data can guide appropriate decision making
|
Presenter:
Nathan Ledeboer, PhD
Professor of Pathology and Vice Chair
Department of Pathology Medical College of Wisconsin
Associate Chief Medical Officer for Laboratory Services
Froedtert Health

Dr. Ledeboer is the director of medical and technical activities for the
Clinical Microbiology and Molecular Diagnostics Laboratories of the
Medical College of Wisconsin. In this role, he oversees development and
implementation of new assays, sign out of all testing performed in these
laboratories, and consults with physician colleagues regarding test
results and selection. |
Using Clinical Breakpoints to Improve Antimicrobial Resistance
Detection
Live Event: Tuesday, December 13, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until June 13, 2023 | Florida Laboratory Credit
available |
|
Antimicrobial resistance (AMR) is an urgent global health threat.
Antimicrobial resistance is detected by clinical laboratories that
perform antimicrobial susceptibility tests (AST) against bacteria
isolated from clinical cultures. AST results are interpreted using
clinical breakpoints, which are updated periodically by standards
development organizations and the U.S. Food and Drug Administration
(FDA). Breakpoint changes can benefit patients and public health only if
adopted in a timely manner by diagnostic companies that develop and
market AST products and/or clinical laboratories that perform AST.
Currently, the United States (U.S.) regulatory framework does not compel
laboratories or diagnostic companies to keep up to date with evolving
AST breakpoints. This results in serious patient safety concerns and
hampers the ability to track and contain the worldwide threat of
antimicrobial resistance.
This presentation will review results from the recent Open Forum
Infectious Diseases publication Raising the Bar: Improving Antimicrobial
Resistance Detection by Clinical Laboraotires by Ensuring Use of Current
Breakpoints. The new College of American Pathologists (CAP) requirements
to ensure breakpoint adherence will be discussed and practical examples
to address these new requirements will be provided. By updating clinical
breakpoints, we can ensure proper patient safety and help detect
antimicrobial resistance to contain the threat.
This webinar will:
•
Define the ongoing pandemic of antimicrobial
resistance
•
Discuss how we can address the ongoing
pandemic in the Clinical Microbiology Laboratory
•
Demonstrate the need to apply updated
clinical breakpoints to interpret antimicrobial susceptibility testing
results
•
Review practical examples on how to update clinical breakpoints to
interpret antimicrobial susceptibility testing results for patient care
|
Presenter:
Patricia (Trish) J. Simner, PhD, D(ABMM)
Associate Professor of Pathology
Director of Bacteriology and Infectious Disease Sequencing Laboratories
Johns Hopkins University School of Medicine

Dr. Trish Simner is an Associate Professor of Pathology and Infectious
Diseases at the Johns Hopkins University School of Medicine and the
Director of the Medical Bacteriology and Infectious Disease Sequencing
Laboratories at the Johns Hopkins Hospital. She completed her PhD at the
University of Manitoba in Manitoba, Canada and a two year Clinical
Microbiology Fellowship at the Mayo Clinic. |
Influenza 2022-2023: Rapid Assessment and Treatment Strategies
Live Event: Thursday, November 17, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until May 17, 2023 | Florida Laboratory Credit
available |
 |
Join this session for the latest insights on global influenza activity
and predictions for the upcoming respiratory season in the Northern
Hemisphere. Influenza diagnostic guidelines and quality initiatives
associated with antimicrobial stewardship and care efficiencies will be
presented. Leaders and members of antibiotic stewardship committees and
healthcare professionals involved in time sensitive and other acute care
areas are encouraged to attend.
This webinar will:
•
Discuss influenza risks and the importance
of an early diagnosis in time-sensitive areas
•
Review IDSA guidelines for diagnosing
influenza
•
Examine accuracy and technology differences
between antigen and molecular tests
•
Explore the impact of an early and accurate
influenza diagnosis on quality of care, infection control, and
stewardship for antibiotics and antivirals

|
Presenters:
 Bruce
Lobaugh, Ph.D., HCLD(ABB) Bruce
Lobaugh, Ph.D., HCLD(ABB)
Director, Central Automated Laboratory
Director, Point-of-Care Testing Program
Administrative Director, Duke University Health System Clinical
Laboratories
Duke University Health System
 Michael
Green MD, MS Michael
Green MD, MS
Associate Medical Director
Assistant Professor - Family Medicine
Zucker School of Medicine at Hofstra/Northwell
|
Value of Point of Care Testing in Diabetes Management
Live Event: Tuesday, November 1, 2022 |
12:00 - 1:00 PM ET
P.A.C.E.®
credit available until May 1, 2023 | Florida Laboratory Credit
available |
 |
The number of adults with diabetes in the world is expected to increase
to 700 million by 2045, including as many as 1 in 3 US adults. Diabetes
leads to changes and symptoms in multiple organ systems. Monitoring and
treating these effectively takes time and attention from the patient and
the healthcare team. Yet most often these patients are seen and managed
in primary care practices who are often under heavy time and cost
containment pressures.
Managing patients diagnosed with diabetes according to the ADA Standards
of Care guidelines is critically important, yet overall testing
compliance is poor. Only 26.7% of patients diagnosed with diabetes meet
targets for glycemic, blood pressure, or cholesterol control.
Several studies suggest that POCT for HbA1c is beneficial in multiple
areas. Outcomes included in these studies suggested patients had greater
understanding and were more satisfied with the state of their disease
and treatment and had better glycemic control. Increased compliance with
ADA testing frequency, improved operational efficiencies and better care
for under-privileged populations have also been observed in studies
investigating POC testing.
This webinar will:
•
Examine the current situation in terms of
diabetes prevalence now and looking towards the future
•
Analyze current guidelines and goals and the
challenges associated with achieving them
•
Review how point of care testing may improve operational efficiencies
and lead to better outcomes

|
Presenter:
Vivian A. Fonseca, MD, FRCP
Professor of Medicine and Pharmacology
Assistant Dean for Clinical Research
Tullis Tulane Alumni Chair in Diabetes
Chief, Section of Endocrinology
Tulane University Health Sciences Center

Dr. Vivian Fonseca, is a Professor of Medicine, Assistant Dean for
Clinical Research, the Tullis-Tulane Alumni Chair in Diabetes, and chief
of the Section of Endocrinology at Tulane University Medical Center in
New Orleans, Louisiana. He is a Past President for Science and Medicine
of the American Diabetes Association (2012), and has served on the ADA
Board of Directors and several committees. |
Science of Tissue Processing: Tidal vs. Rotational Processing
Live Event: Thursday, October 27, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 27, 2023 | Florida Laboratory Credit
available |
 |
Quality sample preparation is fundamental to the analytical process.
Tissue Processing is the most complex and one of the longest steps in the
histology workflow. The quality of the processed specimens will
determine the quality of the stained slides. By reducing processing
times, while increasing tissue quality, a faster diagnosis can be
delivered to the patient, promoting better patient care.
In this webinar, we will review the purpose and function of the steps in
tissue processing, discuss tissue processing reagents, tissue processing
agitation methods, and undercover a way to improve your laboratories
tissue processing methods by using a rotational tissue processor.
This webinar will:
•
Identify the tissue processing steps
•
Choose optimal tissue processing reagents
•
Explain the different tissue processing
methods
•
Compare efficiency of tidal vs rotational
agitation tissue processing
 |
Presenter:
Andrew Lisowski
Senior Technical Content Manager
Epredia

Andrew Lisowski has almost 30 years of experience in histology and
histotechnology. He attended veterinary school and earned his master’s
degree in molecular biology. Andrew worked in histology, IHC and ISH
labs, cell culture lab, performed in-vitro and in-vivo toxicology assays
and was a member of a necropsy team. Currently, Andrew is the Senior
Technical Content Manager at Epredia providing global technical content. |
Workflow Productivity and Sample Security in the Pathology
Laboratory
Live Event: Wednesday, October 26, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 26, 2023 | Florida Laboratory Credit
available |
 |
Pathology laboratories require high quality and reliable sample
identification throughout the possession of patient samples. The
consequence of poor sample identification or non-standard sample
handling can be misidentified samples.
This webinar will discuss common practices such as hand labeling
cassettes and slides and potential downsides of using low-quality
printing printers for items in the lab.
Users will learn what technical details to consider when evaluating
cassette and slide printers in their labs.
This webinar will:
•
Identify potential disadvantages of hand
labeling slides and cassettes
•
Discuss implications of misidentified
samples
•
Examine slide and cassette printer technical
capabilities
•
Analyze laboratory workflows utilizing
cassette and slide printers

|
Presenters:
 Denise
Pernal, HT (ASCP) Denise
Pernal, HT (ASCP)
Field Applications Specialist
Epredia
 Elizabeth
“Buffy” Pancake, MPM, HT (ASCP) Elizabeth
“Buffy” Pancake, MPM, HT (ASCP)
Field Applications Manager
Epredia |
Measuring COVID-19 Immune Response with Ultrasensitive,
PCR-based Neutralizing Antibody Assays
Live Event: Wednesday, October 5, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 5, 2023 | Florida Laboratory Credit
available |
 |
As we look to manage the next phase of the pandemic, it is important to
understand the body’s immune response to SARS-CoV-2 vaccines. Most
antibody testing detects all antibodies in a sample, although only
neutralizing antibodies (NAbs) inhibit the virus from attaching to
cells. Building a complete picture of immune response, including the
role of NAbs, is critical as we face the continued emergence of new
variants.
However, cell-based assays, the current gold standard for SARS-CoV-2 NAb
testing, require additional safety measures for managing live viruses.
These involve long, complicated workflows with poor lab-to-lab
consistency. While some Elisa-based solutions are available, they lack
sensitivity and don’t produce a quantitative measurement.
In this webinar we will learn about a new approach to this problem using
a proprietary method that leverages qPCR to produce quantified NAb
titers.
This webinar will:
•
Explain the importance of NAb testing and the need for standard
testing methods
•
Review current COVID-19 antibody testing options
•
Describe a new technology being used for SARS-CoV-2 NAb testing
•
Explore NAb data for vaccination and emerging variants

|
Presenter:
Feng Xuan, PhD
CTO and Co-founder
Spear Bio

Feng Xuan is the CTO and Co-founder of Spear Bio. Before joining Spear
Bio he was the technology Development Fellow at the Wyss Institute for
Biologically Inspired Engineering at Harvard University. There he
invented Spear Bio’s core technology. Feng received his BS in Chemistry
& M. Phil in Biomedical Engineering from Hong Kong University of Science
and Technology. |
Testing Algorithms Discussion: Preparing for the 2022-23
Respiratory Season
Live Event:
Wednesday, September 28, 2022 |
3:00 - 4:00 PM ET
P.A.C.E.®
credit available until March 28, 2023 | Florida Laboratory Credit
available |
 |
In this webinar, you will learn about the different algorithms available
for COVID-19 testing. The presenters will share the differing opinions
about antigen versus molecular tests and how they may affect patient
care and help limit the spread of SARS-CoV-2. They will also discuss
identifying COVID-19 versus flu due to symptom similarities and how
diagnosis is being managed. Could syndromic panels help distinguish
between the diseases?
Institutions must decide which algorithm works best for them and
consider other important factors for method selection, including cost,
reimbursement potential, and time to result. They must also ask:
• Which
assays will be most effective?
• Will the
test be performed in the laboratory or at the bedside?
•
When should the tests
be performed?
The presenters will offer their opinions on algorithms and why certain
assays are best suited for patient care and disease mitigation. By the
end of the session, you should have a better understanding of the
differences between molecular and antigen testing and how use of either
method could best serve your needs.
This webinar will:
•
Examine the different testing algorithms
that are available for respiratory infections
•
Explain the differences between antigen and
molecular testing and when each type is indicated
•
State the benefits and detriments of
syndromic testing for respiratory targets
|
Presenters:
 Matthew Binnicker, PhD Matthew Binnicker, PhD
Mayo Clinic
Dr. Matthew J. Binnicker is a professor of laboratory medicine and
pathology at the Mayo Clinic in Rochester, Minnesota. He studies viral
infections and new ways to diagnose and manage viral diseases.
Specifically, Binnicker works to develop novel molecular methods to
detect viruses causing respiratory infections and diseases in the
transplant patient population.
 Paul Drain, MD, MPH, FIDSA Paul Drain, MD, MPH, FIDSA
University of Washington
Dr. Paul Drain is an associate professor in the Departments of Global
Health, Medicine (Infectious Diseases), and Epidemiology at the
University of Washington in Seattle. A board-certified physician in
internal medicine and infectious disease, Drain is an attending
physician for the University of Washington Medical Center. |
Use of Automated Next-Generation Sequencing for Rapid Profiling
of Myeloid Malignancies
Live Event:
Wednesday, September 14, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until March 14, 2023 | Florida Laboratory Credit
available |
 |
Modern cancer care relies heavily on biomarker testing for diagnosis of
disease, as well as selection of effective therapies. As the number of
actionable biomarkers continues to increase, single-gene testing methods
have become less practical due to its large specimen requirements, long
turnaround times, and lack of comprehensive coverage, giving rise to
next-generation sequencing (NGS) as a necessary standard of care in
oncology. A sequencing-based approach helps ensure all relevant
biomarkers can be captured at once, making the most of limited sample
tissue while also decreasing critical time-to-results.
Despite the overwhelming need for NGS, many hospitals are reliant on
outsourcing to specialized reference laboratories to perform this
service, leading to long turnaround times for results, and potentially
initiating suboptimal treatment regimens for cancer patients. Recent
advances in automation of NGS, however, have allowed hospitals to bring
this valuable technology in-house, facilitating faster results and
better coordination of care.
In this webinar the speakers will provide a basic overview of NGS
technology and applications, as well as a more detailed experience of
one healthcare institution’s implementation of NGS for myeloid
malignancies.
This webinar will:
•
Review the basic concept of next-generation sequencing (NGS)
•
Identify the primary applications of NGS in precision oncology,
including those for myeloid malignancies
•
Describe how a medical institution implemented NGS testing for
myeloid malignancies in their lab using automated instrumentation
•
Examine how the use of rapid, in-house NGS testing can impact
clinical care for patients with myeloid malignancies
|
Presenters:
 Giovanni
Insuasti, MD Giovanni
Insuasti, MD
Assistant Professor, Pathology
Wake Forest University School of Medicine
Dr. Insuasti is trained in both hematopathology as well as molecular
pathology, with particular interest in myeloid leukemias and
B-lymphocytes.
 Andrew
Hutchison Andrew
Hutchison
Associate Director, Product Management
Thermo Fisher Scientific
Andrew Hutchison is the associate director of product management within
the clinical sequencing division of Thermo Fisher Scientific. Andrew has
served in various scientific, engineering, and product management roles
throughout his career, having a hand in the development of multiple
different sequencing technologies. |
Molecular Testing for Respiratory Tract Infections: Preparing
for an Uncertain Flu Season and the Use of Expanded RTI Panels
Live Event:
Friday, August 19, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until February 19, 2023 | Florida Laboratory Credit
available |
 |
Respiratory tract infections are caused by a variety of viruses,
bacteria, fungi, and other microbes that cause similar symptoms.
Moreover, the concurrent presence of viral and bacterial pathogens is a
growing concern and effective detection methods are required to detect
potential co-infections. The addition of SARS-CoV-2 to the pathogen
ecosystem has further complicated this landscape. Accurate detection of
these pathogens is critical for appropriate patient management and
molecular testing is an extremely sensitive method to achieve this.
In this webinar, the speakers will discuss common questions regarding
expectations for the upcoming flu season, testing for the plethora of
respiratory pathogens capable of causing severe disease, and
antimicrobial stewardship.
This webinar will:
•
Assess the dynamics of the upcoming cold/flu
season and learn about molecular diagnostic solutions for simultaneously
detecting and differentiating COVID-19, seasonal flu, and other
illnesses
•
Clarify the clinical guidelines and value of
expanded molecular panels for identifying influenza-like illnesses,
co-infections, and anti-microbial resistance
•
Prepare to utilize your existing
capabilities to implement molecular testing for respiratory tract
infections in your lab
|
Presenters:
 Manoj Gandhi, MD, PhD Manoj Gandhi, MD, PhD
Sr Director, Clinical
Thermo Fisher Scientific
 Vijay
Singh, MS, PhD Vijay
Singh, MS, PhD
VP, R&D
HealthTrackRx
|
New Perspectives on the Automated Microbiology Laboratory:
Realizing the Potential of Artificial Intelligence
Live Event:
Monday, August 15, 2022 |
4:00 - 5:00 PM ET
P.A.C.E.®
credit available until February 15, 2023 | Florida Laboratory Credit
available |
 |
With requests for “on demand testing” and pressure from clinicians for
rapid turnaround times to the significant and growing shortage of
skilled technologists, microbiology laboratories are increasingly being
asked to do more with less. As a result, juggling various clinical,
operations and financial imperatives is a never-ending task for
laboratory managers as well as the bench.
Ways of driving efficiencies without compromising quality results
represent a significant mitigating factor in this delicate balancing
act. The use of artificial intelligence (AI) and machine learning (ML)
to identify and prioritize clinically-relevant samples is one such tool
that holds the key to streamlining workflows and allowing technologists
to concentrate their skill on what matters most.
This webinar will review the potential that AI and ML offers the
microbiology laboratory, outline currently available solutions that
leverage these advances, and present an overview of the clinical
experience and utility of an in vitro diagnostic device incorporating
machine learning algorithms with digital image capture.
This webinar will:
•
Explain the difference and relationship between artificial intelligence
and machine learning
•
Identify barriers to adoption of this technology in the microbiology
laboratory
•
Review the more recent applications of AI and ML in the microbiology
laboratory
•
Describe the implications of removing negative cultures from a workflow
|
Presenters:
 Steven
Giglio PhD Steven
Giglio PhD
Scientific Director, LBT Innovations
 Rhys
Hill Rhys
Hill
Director of Research, LBT Innovations

Chris Ramsey, PhD Business Development Director, Clever
Culture Systems |
The Impact of Upper Respiratory Infection Testing at the POC:
Speed, Outcomes, and Costs
Live Event:
Wednesday, August 10, 2022 |
2:00 - 3:00 PM ET
P.A.C.E.®
credit available until February 10, 2023 | Florida Laboratory Credit
available |
 |
The COVID-19 pandemic has made an impact on infectious disease testing
and the need to expand testing across the continuum of care. This
webinar will review the benefits of lab centralization and
decentralization, the impact of PCR testing in population health
management, as well as the future of state of upper respiratory testing
in an endemic era.
This webinar will discuss the power of point of care testing for
identification and differentiation of upper respiratory infections and
what role these tests can play in the future. Focusing on how to choose
the right test for the right patient, we will discuss the types of point
of care tests (Rapid Antigen Tests, Lab-based PCR, and Rapid PCR). The
impact of accuracy on patient outcomes, workplace safety and medical
costs.
The benefits of decentralization for timely, actionable results that can
guide treatment decisions during the patient’s first visit. In addition,
Dr. Gupta will discuss how implementing a rapid PCR test impacts
managing community and population health across a healthcare system. As
well as, possible, hurdles and economic factors that come into play when
deciding to implement new testing options.
This webinar will:
•
Assess the benefits of decentralization testing in healthcare systems
•
Describe the future state of upper respiratory testing in post pandemic
and endemic era
•
Identify the value of PCR in patient diagnosis at point of care
•
Explain how to implement Rapid PCR Testing in your health system
|
Presenter:
Dr. Vin Gupta
Assistant Affiliate Professor
Pulmonary/Critical Care Physician
.jpg)
As a Harvard-trained lung specialist, Vin has spent the past 15 years
working worldwide to improve public health for organizations including
the US Centers for Disease Control, the Institute for Health Metrics and
Evaluation, the Harvard Global Health Institute, the World Health
Organization, and the Pentagon’s Center for Global Health Engagement.
Given his diversity of experiences, he is now a trusted advisor and
contributor to national and international media outlets on several of
the most important health issues today, including serving as a regular
health policy analyst for NBC News and contributor to the New York Times
and CNN New Day. |
The Importance of Distinguishing between Aerobic Vaginitis and
Bacterial Vaginosis
Live Event:
Thursday, June 9, 2022 |
2:00 - 3:00 PM ET
P.A.C.E.®
credit available until December 9, 2022 | Florida Laboratory Credit
available |
  |
Vaginal microbiota plays a central role in women’s health and
reproduction. Vaginal microbiota is dynamic, and its bacterial and
fungal community members play a role in its protection. However, these
organisms can also cause vaginal infection if disrupted.
When the vaginal microbiome is disrupted, it creates an opportunity for
protective microbes to decrease and pathogenic microbes to thrive.
Hence, a dysbiotic state, and infections arise. Within infections, there
are those caused by yeasts, which are anerobic and aerobic organisms.
Bacterial vaginosis (BV), which affects 15% of women at reproductive
age, is characterized by anerobic organism dysbiosis.
However, another more recently recognized clinical entity, aerobic
vaginitis (AV), arises with aerobic organism dysbiosis. It is important
to differentiate BV from AV, although sometimes it is not easy with
traditional methods. Unfortunately, AV is sometimes confused with BV. A
diagnostic method based on different bacterial combinations may allow
distinction of BV versus AV, which has clinical significance with
respect to treatment and care. This webinar will present a solution that
could be employed to mitigate misdiagnosis of AV for BV.
This webinar will:
•
Discuss the dynamics involved in the Vaginal
Microbiome
•
Identify the infectious states associated
with vaginal dysbiosis
•
Describe the limitations with traditional
methods for diagnosing infections
•
Propose a molecular testing solution for identifying and
differentiating between pathogenic states of the vaginal microbiota |
Presenter:
Sandeep Mukherjee, MD
Scientific Director, Women’s Health and Infectious Disease, PathGroup
Nashville, Tennessee

Dr. Mukherjee received his PhD in molecular biology from Jadavpur
University in Kolkata, India and performed his fellowship training at
the University of Washington in Seattle. He has been the Scientific
Director of Women’s Health and Infectious Disease at PathGroup in
Nashville, Tennessee since 2014 and has more than 14 years of experience
in molecular diagnostics encompassing women’s health, infectious
diseases, and oncology. |
Top Ten Healthcare Laboratory Safety Hazards
Live Event:
Wednesday, June 1, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until December 1, 2022 | Florida Laboratory Credit
available |
  |
Could you identify the top ten most common hazards in a clinical /
diagnostic laboratory work environment? Compare your list to those from
Dan the Lab Safety Man based on his 30+ years of experience working in,
managing, and leading the Lab’s Safety Programming. You will want to
attend this Webinar to learn about “near misses” in Labs that our
presenter has experienced, addressed and shares with the Safety and
Laboratory colleagues during his experiences touring and inspecting
Clinical Laboratories in Healthcare.
With Dan “The Laboratory Safety Man” Scungio’s help we will identify the
top 10 most frequently seen safety hazards in a healthcare laboratory
and provide cost-effective solutions to avoid these everyday hazards.
Most importantly, our attendees will walk away with a greater
understanding of how they can keep the people around them safe in their
healthcare laboratory.
This webinar will:
•
Outline clear understanding of
basic/intermediate laboratory safety regulations and applications
•
Explain In-depth understanding of specific
lab safety subjects
•
Identify cost effective solutions to these
everyday hazards
•
Adapt a strong ability to relate laboratory
needs to specific lab safety products, PPE, engineering controls, etc
•
Utilize awareness of safety in the healthcare laboratories to drive for
better safety solutions
|
Presenter:
Dan Scungio, MT(ASCP), SLS, CQA(ASQ)
Dan The Lab Safety Man

Daniel J. Scungio, MT (ASCP), SLS, CQA (ASQ) has over 30 years of
experience as a certified Medical Technologist. He has a bachelor’s
degree in Medical Technology from the State University of New York at
Buffalo in Amherst and Buffalo, New York. Dan worked as a laboratory
generalist in hospitals ranging in size from 75 to 800 beds before
becoming a laboratory manager. After 10 years of lab management, he
became the Laboratory Safety Officer for a system of more than 10
hospitals and over 20 laboratories and draw sites in Virginia and North
Carolina. |
Simplifying Group A Streptococci Detection with
Chromogenic Media
Live Event:
Tuesday, April 19, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until October 19, 2022 | Florida Laboratory Credit
available |
  |
Group A Streptococcus (GAS) can cause many different
infections. These infections range from minor illnesses to very serious
and deadly diseases. Each year the testing for Group A Streptococci
(GAS) is growing. Laboratories face continual pressure to turn around
GAS culture results faster while providing accurate results clinicians
can utilize to make informed treatment decisions.
In this webinar, participants will learn how to distinguish growth and
isolation characteristics of GAS using different types of prepared
culture media plates. Furthermore, they will gain insight into the
benefit of using a chromogenic media in the GAS workflow.
Finally, this webinar will present how different types of media perform
within an automation workflow, highlighting technology that can improve
efficiency and productivity in the processing of clinical samples.
This webinar will:
•
Discuss the clinical significance of Group A Streptococcal (GAS)
infections
•
Describe the diagnostic methods currently available for GAS
•
Identify the benefits of chromogenic media for pathogen screening and
diagnostics
•
Review the role laboratory automation can have in improving workflow
productivity
|
Presenters:
 Nathan
Ledeboer, PhD Nathan
Ledeboer, PhD
Medical Director of Microbiology and Molecular Diagnostics, Wisconsin
Diagnostic Laboratories and Froedtert Health
 Matthew
Faron, PhD Matthew
Faron, PhD
Assistant Professor, Medical College of Wisconsin |
Whole Genome Sequencing - Targeted Detection of Resistance Genes
The Complete Spectrum of Clinically Useful
to Clinically Absurd
Live Event:
Wednesday, March 9, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until September 9, 2022 | Florida Laboratory Credit
available |
  |
Antimicrobial resistance poses a significant clinical and public health
burden, with a recent comprehensive assessment estimating global death
rates to be higher than HIV/AIDs or malaria.
Approaches to combat the spread of antimicrobial resistance include,
among other initiatives, a thorough understanding of resistance
mechanisms and the prudent use of antimicrobials.
Whole genome sequencing provides valuable insight into the genetic cause
of resistance and has emerged as a tool to study the emergence and
surveillance of antimicrobial resistance, as well as develop novel
antimicrobials.
While whole genome sequencing has the potential to be used as a clinical
tool to detect the presence of resistance and help guide therapeutic
decisions, antimicrobial susceptibly provides vital information for
optimal clinical management.
This webinar will:
•
Discuss the front-line challenges of multi-drug resistance bacterial
infections from a clinical and laboratory perspective
•
Describe the major recent advances with regard to the detection of
antimicrobial resistance (AMR)
•
Identify the benefits and limitations of the targeted detection of
resistance genes
•
Explain the importance of antimicrobial susceptibility testing in the
clinical management of bacterial resistance
|
Presenters:
 James
A. McKinnell, MD James
A. McKinnell, MD
Associate Professor of Medicine, David Geffen School of Medicine,
University of California, Los Angeles; Division of Infectious Disease,
LA-Biomed at Harbor UCLA Medical Center
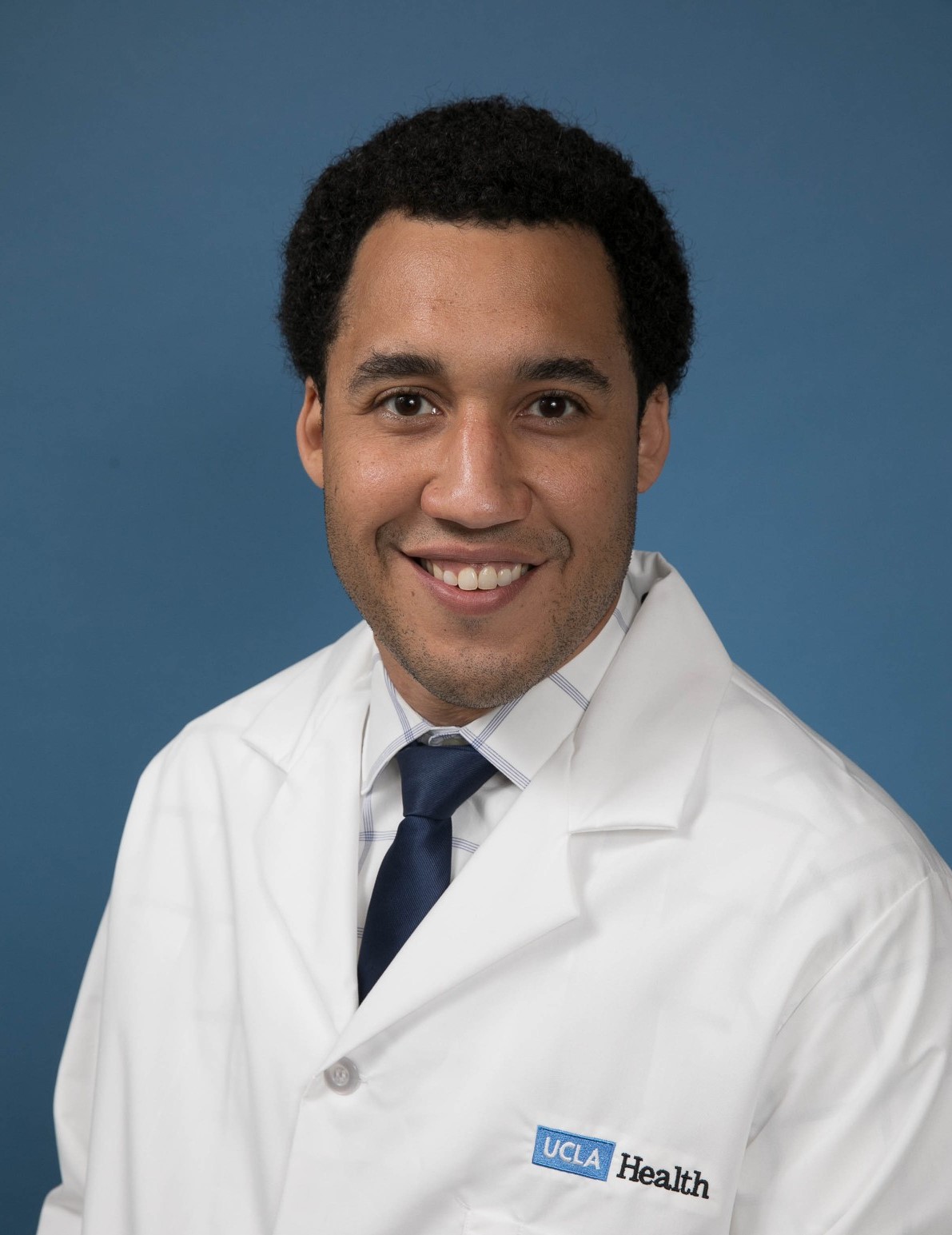 Omai
Garner PhD, D(ABMM) Omai
Garner PhD, D(ABMM)
Associate Clinical Professor, Section Chief, Clinical Microbiology
Director, Point of Care Testing
UCLA Department of Pathology and Laboratory Medicine
|
NSF456-Vaccine Storage: A New Standard Detailing Requirements
for Vaccine Cold Storage
Live Event:
Wednesday, January 19, 2022 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until July 19, 2022 | Florida Laboratory Credit
available |
  |
The World Health Organization estimates that as much as 50% of vaccines
are wasted yearly partly due to incorrect storage temperatures. The
newly launched NSF 456 - Vaccine Storage guideline aims to help vaccine
administrators chose a storage unit that has been certified to stay
within proper temperature to ensure the safety and efficacy of the
vaccines. This session will introduce the new NSF guidelines and how to
evaluate vaccine cold storage products.
This webinar will:
•
Discuss the impacts on the Vaccine Cold Chain in the last 2 years and
its importance
•
Examine the Gaps in the historical Vaccine Storage Recommendations and
how they could lead to wastage or inefficacy
•
Analyze of the NSF standards and how they will improve the vaccine cold
chain
•
Identify other actions in the clinic can help protect vaccines
|
Presenter:
Chase Heibel
Sr. Global Product Manager, Laboratory Refrigeration and Sample
Transport, Thermo Fisher Scientific

Chase Heibel is the Sr. Global Product Manager covering laboratory and
healthcare refrigeration and transport products. He has been with Thermo
Fisher Scientific for nine years where he has held multiple roles
supporting the cold storage business. |
Laboratory Automation in Microbiology: Accelerating the Impact
through AI and Digital Imaging
Live Event:
Thursday, December 16, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until June 16, 2022 | Florida Laboratory Credit
available |
  |
Clinical Microbiology relies on technically skilled laboratorians to
process, and interpret cultures from clinical specimens. Laboratory
automation provides improved accuracy, decreased turnaround times,
improved efficiency and reduced reliance on acquiring, training,and
maintaining a qualified workforce. However, the impact of automation
remains unfulfilled, in part, because robotics fails to incorporate
interpretive processes needed to fully prioritize microbiology work
vital to maximizing efficiencies and accelerating reporting. Experience
from the use of an in-vitro diagnostic device incorporating machine
learning algorithms with digital image capture will be presented.
This webinar will describe the current challenges and drivers within the
microbiology laboratory environment, analyze the bottleneck in various
workflows that heavily rely on skilled labor and examine the downstream
implications of reviewing negative cultures from a workflow.
This webinar will:
•
Describe the current challenges and drivers
within the microbiology laboratory environment
•
Analyze the bottleneck in various workflows
that heavily rely on skilled labor
•
Examine the downstream implications of reviewing negative cultures from
a workflow
|
Presenters:
 Glen
Hansen, PhD, FCCM, D(ABMM) Glen
Hansen, PhD, FCCM, D(ABMM)
Medical Director Microbiology and Molecular Diagnostics
Laboratory
Hennepin County Medical Center
Dr. Glen Hansen is the medical Director of Clinical Microbiology and the
Core Molecular Diagnostics Laboratories at Hennepin County Medical
Center and an Associate Professor in the departments of Pathology &
Laboratory Medicine and Medicine (Infectious Diseases) at the University
of Minnesota.
 Jacqueline
Getty, MLS (ASCP) Jacqueline
Getty, MLS (ASCP)
Microbiology
Hennepin County Medical Center
Jaqueline Getty is a medical technologist at Hennepin County Medical
Center in the department of microbiology. Jaqueline received her MLS
degree from the University of Minnesota. In addition to her clinical
work in microbiology Jacqueline is involved in Hennepin County’s rapid
testing protocols for COVID-19 at the hospital level. |
Combining COVID-19 and Flu Testing to Help Prevent a “Twindemic”
Live Event:
Wednesday, December 15, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until June 15, 2022 | Florida Laboratory Credit
available |
  |
In the age of the pandemic, using one test or the other to “rule out”
one infection is an incomplete and potentially dangerous diagnostic
strategy. Combined rapid antigen testing is the best choice to combat a
‘twindemic’ as it is effective in diagnosing both COVID-19 and the flu
quickly and accurately. Easy-to-use rapid antigen combination tests that
are currently available to clinicians will help facilitate the best
diagnostics possible, leading to faster and more appropriate treatment.
This webinar will describe the continued role antigen testing will play
in managing and ending the COVID-19 pandemic, examine the clinical
overlap between COVID-19, the flu, and other respiratory viruses, and
demonstrate how combined SARS-CoV-2 & Flu A+B testing worksand its
implementation into a facility.
This webinar will:
•
Describe the continued role antigen testing will play in managing and
ending the COVID-19 pandemic
•
Examine the clinical overlap between COVID-19, the flu, and other
respiratory viruses, and how early intervention can reduce the spread
and severity of illness
•
Demonstrate how combined SARS-CoV-2 & Flu A+B testing works, and how to
implement it into a facility
•
Evaluate current patient intake protocols to determine if they are
providing the best treatment possible with an emerging Flu season
 |
Presenters:
 Joseph
Mann, MSN, FNP-C, Global Medical Science Liaison Joseph
Mann, MSN, FNP-C, Global Medical Science Liaison
Integrated Diagnostic Solutions, BD
Joseph Mann is a medical science liaison working in scientific affairs
for Integrated Diagnostic Solutions at BD Life Sciences. He is a board
certified family nurse practitioner licensed in the state of Maryland.
 Megan
Wimmer, Associate Director Megan
Wimmer, Associate Director
Health Economics and Outcomes Research, BD
Megan Wimmer is an Associate Director of Health Economics and Outcomes
Research, with over ten years as part of the BD team advancing the world
of health. Prior to BD, she worked in academia and has specialized
experience in data analysis, computational modeling, epidemiology and
infectious disease. |
Patient Sample Management and Chain of Custody: Modern Practices
for Modern Demands
Live Event:
Tuesday, December 7, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until June 7, 2022 | Florida Laboratory Credit
available |
  |
Pathology and histology laboratory managers are the custodians of vital
patient assets in the form of FFPE tissue blocks and slides generated
from tissue biopsies. In this role, laboratory managers must balance the
demands of federal, state, and local regulations to maintain secure
control over these vital assets with the need to have these assets
accessible for check-out requests.
With cancer cases in particular, biopsied tissue samples are not only
essential in the initial diagnosis, but continue to serve a vital
purpose for those patients seeking to enroll in clinical trials.
Enrolling in these trials can be extremely competitive and
opportunistic, and often requires patients to submit their preserved
tissue samples as part of the qualifying process for acceptance into a
trial. If the sample takes too long to be located, or worse yet go
missing, the patient may miss their chance for enrollment with
potentially disatrous consequences both for that patient’s future and
the reputation of the hospital in charge of maintaining secure custody
of that sample.
In this webinar, we will explore the increasing challenges in
maintaining secure chains of custody and proper asset management
practices for patient tissue samples, three different asset management
models currently in practice, and a case study of Massachusetts General
Hospital’s experience implementing an automated tissue management
system.
This webinar will:
•
Identify the factors that increase the
demand on and complexity of tissue asset management practices
•
Discuss the pros and cons of leading asset
management system methodologies
•
Examine via a case study how a digital tissue archiving solution can
lead to increased security and fewer lost or misplaced samples
|
Presenter:
Joan Vesey, HTASCP
Owner Red Fox Histology Solutions, LLC

Joan is an accomplished histologist with over 30 years of experience in
histology in both the clinical and laboratory setting encompassing
applications, R&D and even owning her own histology consulting company.
Joan helped develop some of the H&E staining consumables we’ve come to
recognize in the industry, and her expertise aligns with Epredia’s
mission and vision to improve lives by enhancing cancer diagnostics. |
Using Procalcitonin to Safely Reduce Antibiotic Use and Improve
Outcomes
Live Event:
Friday, November 12, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until May 12, 2022 | Florida Laboratory Credit
available |
  |
Overuse of antimicrobials is estimated at a rate of 50% in the acute
care setting. It is a practice that has been well documented for more
than thirty years. While most everyone acknowledges this overuse, the
rate has not improved since we began measuring the use of antibiotics.
Overuse can lead to poor patent outcomes, antibiotic resistance,
Clostridioides difficile infections (CDI), longer lengths of stay, more
adverse drug events, increased mortality, readmission, and increased
costs to the patient and hospital.
This is understandable as clinicians tend to “err in favor of caution”.
Clinical symptoms of many diagnoses are similar and it is often
difficult to determine the need for antibiotics based on clinical
presentation, radiology images, and markers other than procalcitonin
(PCT). It is easy to fall prey to prescribing antibiotics “just to be
sure” with the assumption that more is better.
More appropriate prescribing and earlier cessation of antibiotics
enabled by the use of a high sensitive and specific marker like
procalcitonin has been shown in thousands of publications to safely
reduce antimicrobial use while concurrently improving clinical outcomes
and economic burden. This webinar will differentiate the pathophysiology
and kinetics of procalcitonin in comparison to current biomarkers and
establish the role of procalcitonin in antibiotic stewardship.
This webinar will:
•
Differentiate the pathophysiology and kinetics of procalcitonin in
comparison to current biomarkers
•
Establish the role of procalcitonin in antibiotic stewardship
•
Evaluate the expected clinical and financial outcomes of PCT-guided
therapy
|
Presenter:
Dr. Mike Broyles, PharmD

Dr. Broyles has more than 30 years of experience as a Hospital
Pharmacy and Laboratory Director and 28 years consulting for a large IHN
as their Pharmacy Advisory Chairman. Additionally, he has consulted for
more than 25 of the 40 largest integrated health care networks in the
U.S. on antimicrobial stewardship and procalcitonin use. He serves in
antimicrobial stewardship roles for the State of Arkansas, Faculty for
Medscape Infectious Diseases and Medscape Faculty for Biomarkers. |
Clinical Challenges of SARS-CoV2 and Antimicrobial Resistance
Live Event:
Tuesday, October 26, 2021 |
3:00 - 4:00 PM ET
P.A.C.E.®
credit available until April 16, 2022 | Florida Laboratory Credit
available |
  |
COVID-19 has reshaped many aspects of healthcare. Not to be overlooked
is the impact of the pandemic on another major public health threat –
resistant bacterial pathogens. With the documented use of unnecessary
antibiotics early in the course of the spread of the virus, the
abandonment of routine stewardship initiatives in the face of
overwhelmed healthcare systems, and the deprioritization of resistance
surveillance, the threat posed by antimicrobial resistance remains
significant, and may have accelerated.
Multi-drug resistance is challenging for institutions to manage,
particularly if pathogens are transmitted among vulnerable patient
populations. There may be few therapeutic options available, and they
may be further limited by the compromised state of patients. Access to
accurate diagnostic tools that can guide the most appropriate clinical
decisions regarding these life-threatening infections is critical.
Access to accurate antimicrobial susceptibility platforms in
microbiology laboratories — that include drugs of last resort as well as
novel drugs — can lead to more effective and optimal treatment decisions
regarding resistant bacteria, ultimately improving patient outcomes.
This webinar will:
• Discuss the front-line challenges of
COVID-19 from a clinical and laboratory perspective
• Describe the impact of the COVID-19
pandemic on Antimicrobial Stewardship Principles
•
Examine the potential longer-term consequences of a viral pandemic on
emerging bacterial resistance
|
Presenter:
James A. McKinnell, MD
Associate Professor of Medicine, David Geffen School of
Medicine, University of California, Los Angeles; Division of Infectious
Disease, LA-Biomed at Harbor UCLA Medical Center
James A. McKinnell, M.D. is an Associate Professor of Medicine at the
David Geffen School of Medicine at the University of California, Los
Angeles. He is also a member of the Infectious Disease Clinical Outcome
Research Unit (ID-CORE) and the Los Angeles Biomedical Research
Institute at Harbor-UCLA. He is a nationally-recognized infectious
disease specialist with specific research interests related to the
clinical management and prevention of healthcare-associated infections. |
The Future of Next Generation Sequencing in SARS Surveillance
and Precision Oncology
Live Event:
Thursday, October 7, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until April 7, 2022 | Florida Laboratory Credit
available |
 |
The lack of access to SAR-CoV-2 vaccines in much of the world, waning
immunity in vaccinated individuals, vaccine hesitancy, and failure to
follow social distancing and masking recommendations places significant
selective pressure for the continued emergence of SARS-CoV-2 variants of
concern. Coordinated public health efforts to rapidly sequence
SARS-CoV-2 from samples is essential to detect and mitigate their impact
and spread. Utilizing the next gen sequencing, Dr. Leal will describe
how his laboratory was able to rapidly establish viral genome sequencing
and was the first to detect all major variants of concern in the State
of Alabama. The high accuracy, speed, and throughput enables his lab to
provide timely data to guide infection prevention and public health
interventions in his hospital system, region, and State.
Historically, turnaround time for next gen sequencing has been lengthy.
New developments within next-gen sequencing technology have enabled the
turnaround time to be shortened significantly. In addition, the
workflows are much simpler, and labs can be more efficient with
personnel time and lab utilization. Dr. Mackinnon will discuss how these
new advancements are enabling labs who are performing oncology testing
using next gen sequencing. Modern sequencing technology has improved the
operational capacity and efficiency of the lab, due to the low hands on
requirements, rapid turnaround times, and simplified informatics.
This webinar will:
• Describe the current situation around SARS
CoV-2 mutation emergence and why it is important to monitor emerging
variants
• Discuss how the University of Alabama
implemented a next generation sequencing workflow to sequence samples to
monitor the spread of variants across the state of Alabama
• Evaluate how NGS can be used to
successfully perform variant analysis
•
Discuss how the rapid turnaround time of NGS is making an impact
compared to previous more lengthy turnaround times
|
Presenters:
 Sixto
M. Leal Jr., MD, PhD Sixto
M. Leal Jr., MD, PhD
Assistant Professor
Director, Clinical Microbiology, Fungal Reference Laboratory, Department
of Pathology, Division of Laboratory Medicine
UAB Medicine, The University of Alabama at Birmingham
Dr. Sixto Leal received his MD/PhD training in the Medical Scientist
Training Program (MSTP) at Case Western Reserve University, pathology
residency training at the University of North Carolina in Chapel Hill,
and Microbiology fellowship training at the Cleveland Clinic.
 Alexander
Craig Mackinnon, MD, PhD Alexander
Craig Mackinnon, MD, PhD
Director, Genomic Diagnostics and Bioinformatics
University of Alabama at Birmingham
Dr. Alexander “Craig” Mackinnon Jr. is the inaugural director of the
Division of Genomics Diagnostics and Bioinformatics in the Department of
Pathology School of Medicine at the University of Alabama at Birmingham.
Dr. Mackinnon is leading ongoing efforts to establish the Precision
Diagnostic Laboratory at UAB. |
Demystifying the Development and Implementation of Molecular
Tests
in a Clinical Laboratory
Live Event:
Wednesday, September 22, 2021 |
3:00 - 4:00 PM ET
P.A.C.E.®
credit available until March 22, 2022 | Florida Laboratory Credit
available |
  |
Laboratory developed tests (LDTs) have historically been misunderstood
by some due to the perceived complexity of the design and implementation
process. In this webinar, we aim to educate attendees about the overall
process and benefits of LDTs to encourage labs to consider adding
molecular workflows for new applications, now that they are familiar
with qPCR through the pandemic.
We will explain the benefits and help to demystify the process of
implementing LDTs, define what a LDT is, discuss the various ways that
LDTs can be developed, and explain how LDTs differ from IVD/CE-IVD
tests. We’ll also discuss why a lab would want to develop it’s own LDT.
For example, a lab may develop a LDT when there is no test currently
available, such as for rare or new pathogens, including SARS-CoV-2. LDTs
can also reduce the overall cost of performing a test in house. We will
also describe how LDTs are regulated under the Clinical Laboratory
Improvement Act (CLIA), and what the role of government agencies is in
regulating these tests.
This webinar will:
• Describe different types of laboratory
developed tests
• Identify differences between laboratory
developed tests and IVD-R tests
•
List the benefits of running a laboratory developed test
•
Explain how laboratory developed tests are designed and regulated in the
US
|
Presenter:
Mara G. Aspinall
Managing Director, Health Catalysts Group
Professor of Practice, Biomedical Diagnostics
Arizona State University

Mara Aspinall is a healthcare industry leader and pioneer committed to
active civic involvement. She is Managing Director and Co-Founder of
BlueStone Venture Partners. Mara also heads the Health Catalysts Group,
a consulting firm for HIT and Diagnostics, publishing the popular Health
Catalysts Diagnostics Year in Review. |
The Importance of Pediatric Lipid Testing in the Diagnosis and
Treatment of Familial Hypercholesterolemia
Live Event:
Thursday, September 2, 2021 |
1:00 - 2:30 PM ET
P.A.C.E.®
credit available until March 2, 2022 | Florida Laboratory Credit
available |
  |
Familial hypercholesterolemia (FH) is a common genetic disorder leading
to elevated low density lipoprotein cholesterol (LDL-C) from birth1.
Globally out of 220 children, approximately one child has FH, and
therefore an increased risk to suffer from early cardiovascular disease,
or even early death1. One
in ten premature myocardial infarctions (MI) is caused by FH2.
Yet 90% of the 1.3 million Americans with FH are unaware of their
condition, leading to premature atherosclerotic cardiovascular disease
(ASCVD).1,2
The Centers for Disease Control and Prevention (CDC) defines FH as a
Tier
1 genomic application, i.e., having significant potential for positive
impact on public health based on available evidenced-based guidelines
and recommendations3. Yet
implementation of evidenced based practices (EBP) for FH screening is
suboptimal for many reasons, ranging from lack of FH awareness among
both healthcare providers and the public, to the absence of a structured
approach to screening, diagnosis and treatment4-6.
Few health systems have adopted the 2011 recommendations of the National
Heart Lung Blood Institute (NHLBI) and the American Academy of
Pediatrics (AAP) to conduct universal screening of all children between
the ages of 9-117.
Pediatricians often note that they do not routinely send children for
laboratory tests and also state that they feel inadequately prepared to
treat elevated LDL-C levels in children6,8.
In addition to FH education, pediatricians will benefit from point of
care (POC) desktop analyzers for use in their offices.
This webinar will:
•
Describe the specific genetics of FH and the benefits of early treatment
of hypercholesterolemia associated with this genetic disorder1,9
•
Examine the role of cascade screening in the diagnosis of FH1,3,4
•
Identify the barriers to implementing universal pediatric lipid
screening4-6,8
•
Analyze the value of point of care (POC) lipid testing in pediatric
offices – allowing parents and children to avoid a trip to a laboratory
References:
1McGowan
MP, Hosseini Dehkordi SH, Moriarty PM, Duell PB. Diagnosis and Treatment
of Heterozygous Familial Hypercholesterolemia. J Am Heart Assoc
2019;8:e013225.
2Singh A, Gupta A, Collins BL, et al. Familial
hypercholesterolemia among young adults with myocardial infarction. J Am
Coll Cardiol. 2019;73(19):2439-2450.
3CDC. Genomics & Precision Health. Tier 1 Genomic Application
Toolkit for Public Health Departments:
https://www.cdc.gov/genomics/implementation/toolkit/index.htm
accessed January 31, 2021.
4Knowles JW, Rader DJ, Khoury MJ. Cascade Screening for
Familial Hypercholesterolemia and the Use of Genetic Testing. JAMA
2017;318:381-382
5Lee C, Rivera-Valerio M, Bangash H, Prokop L, Kullo I. New
case detection by cascade testing in familial hypercholesterolemia: A
systematic review of the literature. Circ Genom Precis Med.
2019;12:e002723.
6Ferranti SD de et al. Cholesterol Screening and Treatment
Practices and Preferences: A Survey of United States Pediatricians. J
Pediatr 2017;185:99-105
7Expert Panel on Integrated Guidelines for Cardiovascular
Health and Risk Reduction in Children and Adolescents, National Heart,
Lung, and Blood Institute. Expert panel on integrated guidelines for
cardiovascular health and risk reduction in children and adolescents:
summary report. Pediatrics.2011;128(suppl 5):S213-S256
8Dixon DB, Kornblum AP, Ste_en LM, Zhou X, Steinberger J.
Implementation of lipid screening guidelines in children by primary
pediatric providers. J Pediatr 2014;164:572-.
9Luirink IK, Wiegman A, Kusters DM et al. 20-year follow-up
of statins in children with familial hypercholesterolemia. N Engl J Med.
2019;381:1547-56.
|
Presenter:
Mary McGowan, MD
Co-Director
Lipid Clinic at Dartmouth-Hitchcock Heart and Vascular Center
Chief Medical Officer
The FH Foundation

Dr. Mary McGowan is an Assistant Professor of Medicine at The Geisel
School of Medicine at Dartmouth and the Co-Director of the Lipid Clinic
at Dartmouth-Hitchcock Heart and Vascular Center. She is the Chief
Medical Officer of the Familial Hypercholesterolemia Foundation. She is
the author of numerous articles and 5 books. She has been the principal
investigator on over 30 national and international clinical trials and
has lectured widely in the United States, Canada, Europe and Asia on
cholesterol metabolism. |
The Essential Role of Clinical Microbiology in Antimicrobial
Stewardship
Live Event:
Thursday, July 15, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until January 15, 2022 | Florida Laboratory Credit
available |
  |
The incidence of secondary bacterial infections during the COVID-19
pandemic has not mirrored that of past viral pandemics. This likely led
to unnecessary antimicrobial usage, particularly at the onset of the
pandemic. These treatment decisions are not aligned with the antibiotic
stewardship goals, and are associated with the risk of promoting
bacterial resistance and the development of multi-drug resistance
microorganisms (MDRO).
The clinical microbiology lab can effectively support antibiotic
stewardship principles and programs with the appropriate use of
diagnostic testing and timely, clinically-relevant reporting of
susceptibility results to positively impact patient outcomes, resistance
rates and hospital costs.
In this webinar, we will review the impact of COVID-19 on the
microbiology laboratory, antimicrobial resistance, and the effective
management of critically ill patients. It will also review antimicrobial
testing challenges in critically ill patients, examine the impact
clinical microbiology laboratory data can have on accurate treatment
decisions and better management of critically ill patients, and outline
the role the microbiology lab plays to support antimicrobial stewardship
during a pandemic.
This webinar will:
• Examine the impact clinical microbiology
laboratory data can have on accurate treatment decisions and better
management of critically ill patients
• Describe the impact that COVID-19 has had
on antimicrobial resistance
•
Review antimicrobial testing challenges in critically ill patients
• Outline the role the microbiology lab plays to
support antimicrobial stewardship during a pandemic
|
Presenter:
Romney M. Humphries, Ph.D., D(ABMM), M(ASCP)
Professor of Pathology, Microbiology, and Immunology
Medical Director of the Microbiology Laboratory
Vanderbilt University Medical Center

Dr. Romney Humphries, Ph.D., D(ABMM), is a nationally recognized expert
in antimicrobial susceptibility testing antimicrobial resistance (AMR).
With expertise that includes improving the speed and accuracy of
identifying antibiotic-resistant bacteria infecting patients to
investigating novel resistance mechanisms and the evaluation of
therapeutics designed to treat these critical infections, she currently
serves as Medical Director of the Microbiology Laboratory at Vanderbilt
University Medical Center. |
The Importance of Molecular Testing to Detect New
SARS-CoV-2 Mutations
Live Event:
Wednesday, June 16, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until December 16, 2021 | Florida Laboratory Credit
available |
 |
The emergence of novel SARS-CoV-2 variants can have profound effects on
efforts to fight the ongoing pandemic. Besides potentially being more
transmissible or more lethal, emerging variants can affect diagnostic
assays, lead to therapy resistance or reduced effectiveness of vaccines
for corona virus disease 2019 (COVID-19). In this webinar we will
present an overview of approaches for genetic and genomic surveillance a
laboratory can apply depending on the technology and resources
available, in order to detect and discover new mutations in SARS-CoV-2.
The webinar will provide details on the major molecular diagnostic
methods and common molecular viral targets used for testing patients
samples for SARS-CoV-2. We will also discuss the currently circulating
SARS-CoV-2 variants, the mutations that characterize them and their
functional effects on the biology of the virus. Different options for
the detection, discrimination and discovery of emerging SARS-CoV-2
variants using genetic approaches will also be discussed. The webinar
will provide an overview of different strategies such that laboratory
professionals can efficiently utilize precious laboratory resources,
while at the same time being able to successfully scale up surveillance
testing as the world moves from a pandemic to an endemic environment.
This webinar will:
• Describe the major Emergency Use Authorization method
categories used in U.S. clinical laboratories to detect SARS-COV-2 in
patient samples
• Contrast SARS-COV-2 patient testing to testing for the
purpose of surveillance and epidemiology
• Explore the currently circulating SARS-CoV2 variants, the
mutations that characterize them and their functional effects on the
biology of the virus
• Examine different options for the detection, discrimination
and discovery of emerging SARS-CoV-2 variants using genetic approaches
|
Presenters:
 Donna
M. Wolk, MHA, Ph.D., D(ABMM), Geisinger Diagnostic Medicine
Institute, Geisinger Commonwealth School of Medicine Donna
M. Wolk, MHA, Ph.D., D(ABMM), Geisinger Diagnostic Medicine
Institute, Geisinger Commonwealth School of Medicine
Dr. Wolk serves as the Division Director for “Molecular and Microbial
Diagnostics and Development” in the Department of Laboratory Medicine at
Geisinger, an integrated healthcare delivery network serving ~ 3 million
people in Central PA, pioneering the adoption of population health,
precision medicine, and value-based care.
 Jelena
Feenstra, Ph.D. Jelena
Feenstra, Ph.D.
Senior Manager, Global Scientific Communications, Thermo Fisher
Scientific
Dr. Feenstra has extensive diagnostic and research experience in
genetics, cytogenetics and genomics. She has a PhD in experimental
Oncology from the Medical University of Vienna, and has previously
worked as a Senior Scientist at the Ludwig Boltzmann Institute in
Vienna. |
Six Steps to an Effective Lockout Program within Healthcare Labs
and Facilities
Live Event:
Tuesday, May 25, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
credit available until November 25, 2021 | Florida Laboratory Credit
available |
  |
Whether you are in a healthcare laboratory or facility, OSHA’s Control
of Hazardous Energy regulation requires that energy sources must be
contained during servicing and maintenance to ensure worker safety.
Safety programs and procedures are many times not on top of mind in the
healthcare labs, even though they are held to the same OSHA standards as
the the maintenance areas. Energy sources that are found both inside and
outside of the healthcare labs can include electrical, mechanical,
hydraulic, pneumatic, chemical, thermal or other sources in machines and
equipment. When such hazardous energy sources are not properly
controlled, workers servicing or maintaining the machines or equipment
may end up seriously injured or even killed.
The regulatory standard (29 CFR 1910.147) also requires that: “The
employer shall establish a(n) (energy control) program consisting of
energy control procedures, employee training and periodic inspections to
ensure that before any employee performs any servicing or maintenance on
a machine or equipment where the unexpected energizing, startup or
release of stored energy could occur and cause injury, the machine or
equipment shall be isolated from the energy source and rendered
inoperative."
Year after year, lockout tagout compliance continues to appear on OSHA’s
Top 10 Cited Standards list. The majority of those citations are due to
a lack of proper lockout procedures, program documentation, periodic
inspections or other procedural elements. This webinar will examine
OSHA’s requirements for your lockout program and why it’s important for
healthcare labs and facilities, identify the 6 Steps to an Effective
Lockout Program for Healthcare Labs and Facilities, discuss the common
failures or complacency that may exist in a program’s present state, and
more.
This webinar will:
• Examine OSHA requirements for your
lockout program and why it’s important for healthcare labs and
facilities
• Identify the 6 Steps to an Effective
Lockout Program for Healthcare Labs and Facilities
•
Discuss the common failures or complacency that may exist in a program’s
present state
• Review best practices for
starting/refreshing a Lockout Tagout program through standardization
|
Presenters:
Carlos Soria
Product Manager, Brady’s Lockout Tagout Devices & Padlocks

Ben Caccese
Product Manager, Brady’s Lockout Tagout Devices & Padlocks
 |
Community Acquired Pneumonia:
Diagnosis and Treatment During the COVID-19 Era
Live Event:
Tuesday, January 26, 2021 |
1:00 - 2:00 PM ET
P.A.C.E.®
& AARC
credit available until July 26, 2021 | Florida Laboratory Credit
available |
  |
This PACE and AARC accredited webinar focuses on community acquired
pneumonia (CAP) and two important pathogens that cause pneumonia. S.
pneumonia is the leading cause of CAP. Legionella causes Legionnaires’
Disease, a severe form of pneumonia that has increased 9-fold since year
2000 in the United States. In light of COVID-19 related temporary
shutdowns of businesses and buildings, the risk of for growth and spread
of Legionella is of heightened concern.
In the laboratory, urinary antigen testing (UAT) provides an alternate
diagnostic path to identify pneumonia etiologies without disrupting
respiratory testing workflow during respiratory season. The practical
utility of pneumonia diagnosis, the use of UAT and their impact will be
discussed.
Join this expert discussion to explore the challenges of managing
pneumonia during the COVID-19 era, and the value of UAT from an
evidence-based and Infectious Diseases Society of America / American
Thoracic Society (IDSA/ATS) guidelines-supported expert assessment for
clinical and laboratory professionals.
This webinar will:
• Describe the relationship of COVID-19
and pneumonia and the associated public health risks
•
Examine experiences and best practices for
evaluating and managing COVID-19 patients with pneumonia
•
Explain the guidance and practical clinical value
of UAT, including mortality reduction and antibiotic stewardship
•
Discuss UAT performance characteristics and
potential value related to laboratory workflow in times of strained
respiratory testing resources |
Presenter:
Antonio Anzueto, MD
Professor, Department of Medicine University of Texas San Antonio and
Chief, Pulmonary Section, South Texas Veterans Health Care System
Dr. Anzueto is Chief in the pulmonary section of The South Texas
Veterans Health Care System, Audie L. Murphy Memorial Veterans Hospital
Division in San Antonio, Texas, where he also serves as Medical Director
of the Respiratory Therapy Department and Medical Director of the
Pulmonary Function Laboratory. He is also a professor in the department
of medicine at the University of Texas Health at San Antonio. |
The Essential Role of Clinical Microbiology in
Antimicrobial
Stewardship
Live Event:
Thursday, December 10, 2020
|
2:00 - 3:00 PM ET
PACE®
credit available until June 10, 2021 | Florida Laboratory CE Credit
available |
  |
The principle problem that exists is not about what Antimicrobial
Stewardship is, but more about what data the microbiology lab to is able
to deliver that will support and enhance the overarching goals of the
program for the institution. A lack of alignment can prevent investment
in new methods, access to new therapeutics and effective management of
the most critically ill patients. The platforms that can be used in the
microbiology laboratory and collaboration between stewardship programs
and the microbiology lab can ensure susceptibility testing data is
leveraged to optimize treatment decisions, reduce length of stay and
adverse effects. This will also improve patient safety and outcomes
particularly in critically ill patients.
This webinar will discuss the role the microbiology lab should play to
help ensure that antimicrobial stewardship programs are successful,
identify core elements of microbiology laboratory testing and reporting
that promote stewardship, and illustrate how microbiology lab data can
positively influence clinical decisions.
This webinar will:
•
Discuss the role the microbiology lab should play to help ensure that
antimicrobial stewardship programs are successful
•
Identify core elements of microbiology laboratory testing and reporting
that promote stewardship
•
Illustrate how microbiology lab data can positively influence clinical
decisions
•
Describe the antimicrobial therapy challenges for core stewardship
stakeholder that critically-ill patients pose
|
Presenter:
Romney M. Humphries, Ph.D., D(ABMM), M(ASCP)
Professor of Pathology, Microbiology, and Immunology
Medical Director of the Microbiology Laboratory
Vanderbilt University Medical Center

Dr. Romney Humphries, Ph.D., D(ABMM), is a nationally recognized expert
in antimicrobial susceptibility testing antimicrobial resistance (AMR).
With expertise that includes improving the speed and accuracy of
identifying antibiotic-resistant bacteria infecting patients to
investigating novel resistance mechanisms and the evaluation of
therapeutics designed to treat these critical infections, she currently
serves as Medical Director of the Microbiology Laboratory at Vanderbilt
University Medical Center. |
Using Biomarkers to Inform COVID-19 Treatment
Live Event:
Tuesday, December 8, 2020
|
1:00 - 2:00 PM ET
PACE®
credit available until June 8, 2021 | Florida Laboratory CE Credit
available |
  |
Infection with SARS-CoV-2 results in COVID-19. This infection has
systemic manifestations, including acute lung injury, cardiac damage,
and in rare cases a Kawasaki disease-like illness. With rising cases of
COVID-19 nationally, clinicians benefit from tools to assist decisions
regarding triage, advanced imaging, and treatment decision making.
Biomarker testing has emerged as a potentially useful tool to facilitate
clinical decision making. Biomarker testing may inform risks in patients
with COVID-19, prognosticating poor outcome and as such be helpful to
decide on where patients are admitted (e.g. medical floor vs ICU), how
they are imaged, and whether to apply more advanced treatments.
In this discussion, review of data will focus on use of troponins,
natriuretic peptides, and other biomarkers in a clinically-focused
synthesis of how biomarkers might be used in COVID-19.
This webinar will:
•
Examine the causes of cardiac injury in COVID-19
•
Describe the relationship of the development of a Kawasaki disease-like
illness to COVID-19
• Identify biomarkers with potential utility in COVID-19
•
Develop a strategy to utilize biomarkers to facilitate clinical care in
COVID-19
|
Presenter:
James Januzzi, MD
Hutter Family Professor of Medicine
Harvard Medical School

Dr. Januzzi is a member of the Cardiology Division of the Massachusetts
General Hospital and the Hutter Family Professor of Medicine at Harvard
Medical School. He is an accomplished clinician and clinical trialist,
with a research focus on biomarker testing in cardiovascular disease. He
has more than 650 publications and is an editor at two journals from the
American College of Cardiology journals. |
Point of Care Molecular Testing: Streamlining Cancer Care from
the Anatomic Pathologist’s Office
Live Event:
Wednesday, December 2, 2020
|
1:00 - 2:00 PM ET
PACE®
credit available until June 2, 2021 | Florida Laboratory CE Credit
available |
  |
Delays in biomarker test results can have adverse affects on the
outcomes for cancer patients. Often times, the biomarker report is
delivered back to the oncologist long after the patient begins
treatment. It is common for patients to not only miss out on treatment
opportunities, but also to be prescribed the wrong treatment if the
oncologist does not receive the molecular data in time. With the latest
advancements in next-generation sequencing (NGS), it is now possible to
get full molecular results as quickly and easy as you get your
immunohistochemistry (IHC) results today.
Attend this event to hear first-hand how physicians at William Osler
Health System in Brampton, Ontario are leveraging in-house NGS testing
to deliver better cancer care to patients and improve the outcomes of
their system. By doing so, oncologists receive the genomic testing
results faster and are able to ensure they are prescribing the most
appropriate treatment for the patient.
This webinar will:
•
Describe the role of ancillary biomarker testing in the treatment of
cancer patients
•
Analyze how delays in test results can adversely affect cancer care
•
Identify areas within your own lab or network that impede biomarker
results
•
Explore how existing and novel techniques can help support oncology
practice within your center
|
Presenters:
 Brandon
Sheffield, MD, FRCPC Brandon
Sheffield, MD, FRCPC
Physician Lead of Research, Anatomical Pathologist
William Osler Health System
Dr. Sheffield is an anatomic and molecular pathologist. He is
currently serving as the Medical Director of
Immunohistochemistry and Molecular Pathology, and the Physician
Lead of research for William Osler. |
|
 Parneet
Cheema, HBSC, MD, BIOTECH, FRCPC Parneet
Cheema, HBSC, MD, BIOTECH, FRCPC
Corporate Division Head Medical Oncology/Hematology
William Osler Health System
Dr. Parneet Cheema is an Assistant Professor, at the University
of Toronto, and Head of Medical Oncology/Heamatology and cancer
research at the William Osler. She is an internationally known
expert in lung cancer and precision cancer care in which she has
conducted numerous clinical trials and published national
consensus statements. |
|
Leading Edge SARS-CoV-2 Testing
Live Event:
Monday, November 30, 2020
|
2:00 - 3:00 PM ET
PACE®
credit available until May 30, 2021 | Florida Laboratory CE Credit
available |
  |
As many continue to tackle the day to day battle against COVID-19
disease it is critical that we share the latest leading insights for
this virus, collectively ensuring learning for all. This webinar will be
a scientific exchange of insights from a leading expert in his field.
Helping share a detailed overview of the current known information on
the disease and exploring the variety of diagnostics that can be used to
understand prevalence. The discussion will conclude with thoughts on the
upcoming winter season and how the management of Flu and COVID-19 will
be at the forefront of healthcare challenges in the coming months and
how leading edge technology and thinking may be the only route to
success, helping to save lives and protect communities.
This webinar will:
• Identify what we know to date about
COVID-19 & SARS-CoV-2
• Discuss the forecasted impact of the
disease
• Assess treatment options for COVID-19
• Explain the role of diagnostics and
available diagnostic options
• Describe Flu vs COVID-19
•
Explore insights that help to inform the next 12 months
|
Presenter:
Jeff Andrews, MD, FRCSC
Worldwide Medical Director
Molecular Diagnostics & Women’s Health and Cancer, BD Integrated
Diagnostic Solutions
BD Life Sciences
Jeff Andrews, MD, FRCSC is the Worldwide Medical Director for Women’s
Health and Cancer, BD Life Sciences. A Board-Certified Obstetrician and
Gynecologist, Dr. Andrews has provided care in community settings in
both metropolitan Toronto, Ontario, Canada and Washington, DC. He has
also provided care in academic settings as an Associate Professor at
Duke University Medical Center and at Vanderbilt University Medical
Center. |
Taking a Systematic Approach to Drive Behavior Change in
Diabetic Patients
Live Event:
Wednesday, November 4, 2020
|
1:00 - 2:00 PM ET
PACE®
credit available until May 4, 2021 | Florida Laboratory CE Credit
available |
  |
Diabetes remains a major focus for healthcare providers and chronic
disease management programs. Over 29 million people in the U.S has
diabetes1, with 33–49% of
patients not meeting targets goals for A1C, blood pressure and
cholesterol2. However, a
major barrier to optimal care is a delivery system that is often
fragmented, lacks clinical information capabilities, and is poorly
designed for the coordinated delivery of chronic care.
Successful diabetes care requires a systematic approach to supporting
patients’ behavior change efforts, including the utilization of
multi-disciplinary care teams, personalized provider feedback,
continuous real-time monitoring, and decision support tools to target
and care for patients at risk for poor outcomes.
Ultimately, healthcare institutions are looking for ways to tailor
population care to meet individual patient needs, through integrated
technologies that help to optimally manage and prevent diabetes in the
future. Join Abbott, with Dr. Chad Malone, and learn how to drive
clinical practice to standards that provide the best outcome for
pre-diabetic, and diabetics populations.
1
https://care.diabetesjournals.org/content/39/Supplement_1/S6. Accessed
9/30/2020.
2
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5536329/. Accessed
9/30/2020.
This webinar will:
• Create a health care delivery systems that can proactively identify
your diabetes populations and provide them with evidence-based
patient-centered care
• Empower your patients to feel like the most important part of their
care team by creating a complete picture of their diabetes in the
context of their life, enabling personalized lifestyle and treatment
changes
• Form a complete picture of your diabetic population, and identify gaps
in population management as well as individual outcomes
• Enable a continuous model of chronic disease management and
efficiently achieve quality measures
This session is sponsored by: |
 |
|
Presenter:
Chad Malone, MD
Director, Global Medical Information and Clinical Excellence Solutions
Abbott

Dr. Chad Malone has 25 years of digital healthcare entrepreneurship
within clinical and translational sciences. He graduated from Brigham
Young University with a degree in Japanese; holds an M.D. from Ross
University School of Medicine and performed a residency in Anesthesia at
the University of Rochester.
|
Importance of Sample Collection and Transport In the Age of COVID-19:
Virology and Bacteriology Aspects
Live Event:
Tuesday, June 9, 2020
|
1:00 - 2:00 PM ET
PACE®
credit available until December 9, 2020 | Florida Laboratory CE Credit
available |
  |
For diagnostic testing, proper sample
collection and transport play a pivotal role in the accurate and timely
identification of a pathogen. When testing for respiratory virus, the
gold standard for sample collection is a specialized flocked swab used
to collect a sample from the nasopharynx, which is then transported in
viral transport media.
At the beginning of 2020, swab specimen collection became a household
topic as the Coronavirus (COVID-19) unleashed a global pandemic.
Researchers, assay manufacturers, FDA and CDC considered the different
types of swabs and transport media which could be used to sample
collection and transport for COVID testing.
In this webinar, we will take an in-depth look at specimen collection
swabs, the quality procedures required for manufacturing, the different
types and how they are used to collect samples. We’ll explore guidance
from FDA and CDC on the recommended swabs, collection sites and
transport media, how these recommendations evolved over the weeks during
the pandemic, and role that self-collection will play in the future of
respiratory viral testing.
This webinar will:
• Identify the types of swabs which are commonly used for sample
collection for respiratory viruses and describe the differences between
each
• Describe the types of transport media which are commonly used for
sample collection for respiratory viruses and the differences between
each
• Examine the 4 key factors which make up a good respiratory specimen
for viral detection
• Discuss the evolution of swabs and transport media for respiratory
viruses and the importance of materials, biocompatibility and QC in the
downstream
|
Presenter:
Susan Sharp, PhD., (D)ABMM, (F)AAM, MS, MT(ASCP)
Scientific Director
Copan Diagnostics, Inc.

Dr. Sharp has been a clinical microbiologist and a very active member of
The American Society for Microbiology (ASM) for 30 years serving on
various boards and committees. She is a Diplomat of the American Board
of Medical Microbiology (ABMM) and a Fellow in the American Academy of
Microbiology. She is also an active member of the Board of Scientific
Councilors for the Office of Infectious Diseases of the Centers for
Disease Control and Prevention, and a member of the College of
Pathologists Microbiology Resource Committee. Dr. Sharp is a
Past-President of ASM and a former member of ASM’s Board of Directors. |
How Culture Media Can Deliver Value to Your Lab
Live Event:
Monday, March 16, 2020
|
2:00 - 3:00 PM ET
PACE®
credit available until September 16, 2020 | Florida Laboratory CE Credit
available |
 |
While performance standards of prepared culture media are consistent
among various manufacturers, when sourcing items from a new supplier,
laboratory personnel may find that the general attributes of both the
media and microorganisms differ. In this webinar, Nathan Ledeboer, PhD,
will teach participants how to distinguish growth and isolation
characteristics of normal flora and pathogens between two leading
suppliers of prepared media plates: Thermo Scientific™and BD.
Additionally, Ledeboer will present the physical differences of
enrichment, selective, and differential media available from the two
manufacturers through side by side comparisons. He will also address the
growing impact of automation on the microbiology laboratory by
discussing a case study that highlights new and evolving technologies to
improve efficiency and productivity in the processing of clinical
samples.
This webinar is designed to designed to provide the lab professional
with the skill and insight to effectively handle the implementation of
Thermo Scientific microbiology prepared media by reviewing several
critical aspects to onboarding a new prepared media supplier, including
common procedures and policies for adopting new media and impact to
workflow, ordering, delivery, and media storage and handling.
This webinar will:
•
Explain differential identification of organisms on plates originating
from different manufacturers
•
Discuss the differences in plate composition and construction using the
new plate technology
•
Examine the differences in morphology in the presentation of organisms
on plates
•
Discuss about advances in clinical microbiology using automation
|
Presenters::
 Dr.
Nathan Ledeboer Dr.
Nathan Ledeboer
Medical Director of Microbiology and Molecular Diagnostics for
Wisconsin Diagnostic Laboratories and Froedtert Health
In his role at Medical College of Wisconsin, Dr. Ledeboer
oversees development and implementation of new assays, sign out
of all testing performed in these laboratories, and consults
with physician colleagues regarding test results and selection. |
|
 Brittney
M. Bunn, PhD Brittney
M. Bunn, PhD
Service Support Supervisor, Thermo Fisher Scientific
Dr. Brittney M. Bunn obtained her Ph. D. in chemistry from Case
Western Reserve University. She currently serves as a Service
Support supervisor for Thermo Fisher Scientific and has held
other roles in the Technical Service department during her
tenure of four years. |
|
The Impact of Rapid Molecular Panel-based Testing for Urinary
Tract Infections
Live Event:
Thursday, February 27, 2020
|
1:00 - 2:00 PM ET
PACE®
credit available until August 27, 2020 | Florida Laboratory CE Credit
available |
 |
This webinar will focus on recently published data demonstrating the
clinical impact of molecular tests in Urinary Tract Infections have
traditionally been diagnosed based on culture-based microbiology tests –
which take a long time to result, can lack sensitivity and specificity,
and are prone to contamination. In the last 18 months, the first
commercially available molecular tests for Urinary Tract Infections were
made available to laboratories – providing large amounts of data on the
impact of these tests on UTI testing. In this webinar, we will provide
the latest clinical, economic, and laboratory impact data as a result of
introducing molecular panel-based testing.
The webinar will also address problems and limitations of culture-based
testing for urinary tract infection (UTI), provide an update on clinical
trials and rapid molecular testing for UTIs in practice, and discuss the
economic impact of molecular testing for UTIs.
This webinar will:
•
Identify the problems and limitations of culture-based testing for
urinary tract infection (UTI)
•
Describe the current clinical trials and trends
rapid molecular testing for UTIs in practice
•
Examine the economic impact and reimbursement
trends in molecular testing for UTIs
To access the white paper, "Using
Flexible-Content Syndromic Panels to Help Manage Infectious Disease:
Update on Laboratory Trends and Health Outcomes"
CLICK HERE. |
Presenters:
 David
Baunoch, PhD David
Baunoch, PhD
President and CEO
Pathnostics
Dr. Baunoch has more than 25 years of laboratory experience in a
number of areas and has produced over 25 peer-reviewed
publications. |
|
 Trisha
Lauterbach, MSA, MLS (ASCP), CHT (ASHI) Trisha
Lauterbach, MSA, MLS (ASCP), CHT (ASHI)
Dir., Laboratory Operations
Capstone Healthcare
As the Director of Laboratory Operations at Capstone Healthcare,
Trisha Lauterbach is applying her expertise in clinical
molecular testing to improve patient care and outcomes in
diverse healthcare settings and patient populations. |
|
The Key to Successful Antimicrobial Stewardship:
Interdisciplinary Teams
Live Event:
Wednesday, January 22, 2020
|
1:00 - 2:00 PM ET
PACE®
credit available until July 22, 2020 | Florida Laboratory CE Credit
available |
 |
New drug development has been in decline and antimicrobial resistance
has been steadily on the rise. This dynamic has resulted in the
development of multi-drug resistant microorganisms (MDRO) and challenges
in managing the resulting complicated infections. Antimicrobial
Stewardship Programs have key objectives to promote the appropriate use
of antimicrobials, improve patient outcomes, reduce microbial resistance
and decrease the spread of infections caused by MDROs.
Multi drug resistance is particularly challenging for institutions to
manage, particularly if they are transmitted among vulnerable patient
populations. Optimal therapeutic options may be few and further limited
by toxicity that can further compromise patients. Accurate diagnostic
tools that can guide the most appropriate clinical decisions in these
life-threatening infections are critical.
Microbiology laboratories with access to accurate antimicrobial
susceptibility platforms that include drugs of last resort as well as
novel drugs can lead to more effective and optimal treatment decisions,
reducing cost of stay and improving patient outcomes.
This webinar will:
•
Discuss how current budgeting practices
between the microbiology laboratory, the pharmacy, and the hospital has
created some bizarre incentives that can impact the practice of
antibiotic stewardship.
•
Explain how creative approaches to the use
of older antibiotics might either harm or benefit patients.
•
Explain how microbiology laboratories with access to accurate
antimicrobial susceptibility platforms, including drugs of last resort
as well as novel drugs can lead to more effective and optimal treatment
decisions, reducing cost of stay and improving patient outcomes.
|
Presenter:
James A. McKinnell, MD
Assistant Professor of Medicine
David Geffen School of Medicine, University of California, Los Angeles
James A. McKinnell, M.D. is an Assistant Professor of Medicine at the
David Geffen School of Medicine at the University of California, Los
Angeles. He is also a member of the Infectious Disease Clinical Outcome
Research Unit (ID-CORE) and the Los Angeles Biomedical Research
Institute at Harbor-UCLA. He is a nationally-recognized infectious
disease specialist with specific research interests related to the
clinical management and prevention of healthcare-associated infections. |
Procalcitonin Aided Antibiotic Stewardship: The New Paradigm
Live Event:
Thursday, December 5, 2019
|
1:00 - 2:00 PM EST
PACE®
credit available until June 5, 2020 | Florida Laboratory CE Credit
available |
 |
Signs and symptoms of bacterial, viral infection and non-infectious
diagnosis overlap lack of specificity in most biomarkers cause many
prescribers to give antibiotics erring in favor of caution or "just to
be sure". Statistically up to 50% of antibiotics prescribed in hospitals
are unnecessary. Overprescribing antibiotics has led to resistant
bacteria which is making it harder to treat.
Procalcitonin can aid in severity assessment and evaluation of therapy
choices, and attendees will gain an understanding of the role of
procalcitonin in antibiotic stewardship as well as the expected clinical
and health economic outcomes of procalcitonin guided therapy.
This webinar will describe the pathophysiology and kinetics of
Procalcitonin during sepsis and infection and discuss the concept of
Procalcitonin-aided antibiotic stewardship in sepsis and low respiratory
tract infections. It will also compare and contrast the costs and
outcomes with PCT-aided antibiotic therapy decisions compared to
standard care in specific published patient population studies and
summarize the most impactful cost components and value drivers of PCT
testing.
This webinar will:
•
Describe the pathophysiology and kinetics of
Procalcitonin during sepsis and infection
•
Discuss the concept of Procalcitonin-aided
antibiotic stewardship in sepsis and low respiratory tract infections
•
Compare and contrast the costs and outcomes
with PCT-aided antibiotic therapy decisions compared to standard care in
specific published patient population studies
•
Summarize the most impactful cost components and value drivers of PCT
testing
This session is sponsored by: |
 |
|
Presenter:
Michael R Broyles, BSPharm, RPh, PharmD
Director of Pharmacy and Laboratory Services
Five Rivers Medical Center, Pocahontas, Arkansas

Mike Broyles, PharmD, is director of pharmacy and laboratory services at
Five Rivers Medical Center in Pocahontas, Arkansas. He received his
BSPharm degree in pharmaceutical sciences from the University of
Missouri-Kansas City and his PharmD from the University of Arkansas for
Medical Sciences. With more than 25 years of experience as a hospital
pharmacy director and laboratory director, Mike enjoys educating
patients on current concepts in the clinical use of drugs. |
Capillary Electrophoresis: Genetic Disease Testing for
Challenging Targets in the Modern Clinical Lab
Live Event:
Thursday, October 31, 2019
|
1:00 - 2:00 PM EST
PACE®
credit available until May 1, 2020 | Florida Laboratory CE Credit
available |
 |
The fast-paced development of new sequencing technologies offer rapidly
growing options for molecular testing of genetic disorders. This can
make it challenging for clinical labs to offer the best diagnostic
technology or assay for the many diverse diagnostic scenarios they face.
One of the key advantages of capillary electrophoresis versus
next-generation sequencing is its capability to sequence difficult
regions specifically long, repeat expansion DNA sequences and copy
number variants as observed in neurological disorders such as Fragile X
Syndrome and Spinal Muscular Atrophy (SMA).
With rising awareness of genetic diseases and personalized medicine,
testing for these disorders is becoming increasingly important for
diagnosis and genetic screening in newborns and disease carriers in
expecting parents. This trend that will no doubt continue as targeted
genetic therapies, like those recently approved for SMA, are developed
for other genetic diseases.
This webinar will discuss the basics of capillary electrophoresis as a
platform for DNA analysis in a modern clinical laboratory. By coupling
this platform with novel PCR methods, we will demonstrate how this
technology can be used screen and diagnose disorders associated with
challenging repetitive DNA and copy number variants.
This webinar will:
•
Evaluate the strengths and weaknesses of capillary electrophoresis for
nucleic acid diagnostics compared to other methods
•
Describe the importance of genetic disease testing for carrier screening
and newborn screening applications
•
Discuss how the roles of capillary electrophoresis and genetic disease
testing have changed over time—and how they might change in the future
|
Presenter:
John N. Milligan, Ph.D.
Senior Scientist, Product Development
Asuragen

Dr. Milligan is a Senior Scientist in product development at Asuragen in
Austin, TX, where he develops and validates assays for the testing of
hereditary and oncological genetic diseases. He earned his doctorate in
Molecular Biology at the University of Texas, where his work focused on
point of care diagnostics and protein engineering, including engineering
a novel polymerase for use with isothermal amplification and strand
displacement applications. |
Mitigating the Risk of Bacterial Contamination of Platelets:
Recent Developments
Live Event:
Monday, October 21, 2019
|
8:15 - 9:15 AM EST
PACE®
credit available until April 21, 2020 | Florida Laboratory CE Credit
available |
 |
If you won't be attending the 2019 American Association of Blood Banks
annual meeting in San Antonio this year, we have you covered! This
webinar will be held in conjunction with a live conference at AABB (thus
the early start). Join us for a session that will cover the latest
developments and the recommendations in the FDA Final Guidance that will
define how blood collection centers and hospital blood banks and
transfusion services will need to operate moving forward.
This webinar will identify the extent and nature of the risk for
bacterial risk in platelets and review FDA final guidance and the
options for addressing this risk and their implications. It will also
describe the role of rapid testing in satisfying the FDA guidance and
discuss recent advances in rapid testing technology for bacteria in
platelets. Learn how you can take advantage of the latest science to
most cost-effectively meet the requirements of the new FDA Final
Guidance.
This webinar will:
•
Identify the extent and nature of the risk for bacterial risk in
platelets
•
Review FDA Final guidance and the options for addressing this risk and
their implications
•
Describe the role of rapid testing in satisfying the FDA guidance
•
Discuss recent advances in rapid testing technology for bacteria in
platelets
This session is sponsored by: |
 |
|
Presenter:
Michael R. Jacobs, MD, PhD
Professor Emeritus, Department of Pathology,
Case Western Reserve University;
Director Emeritus, Clinical Microbiology,
University Hospitals Cleveland Medical Center

Dr. Jacobs is a world renowned expert on the risks of bacterial
contamination in platelet components. He has published landmark research
on this topic and has been a leader in improving public health by
shaping clinical practices and policy in this area. |
Antimicrobial Stewardship and the Role of Improved Diagnosis in
the Management of Acute Respiratory Tract Infections
Live Event:
Tuesday, September 17, 2019
|
1:00 - 2:00 PM EST
PACE®
credit available until March 17, 2020 | Florida Laboratory CE Credit
available |
 |
Acute respiratory tract infections (ARI) are a very common clinical
presentation, and one of the main drivers of antimicrobial prescribing
in adults and children. Many (perhaps the majority) antibiotic
prescriptions are thought to be inappropriate, driving antibiotic
resistance, adverse effects from antibiotics, and care seeking
behaviors.
Improved diagnostic accuracy is one major strategy for better targeting
the use of antibiotics and antivirals. For ARI there are two main groups
of diagnostic tests (above and beyond clinical features, which alone are
not reliable): tests to detect pathogens in respiratory samples, and
tests that try to assess the body’s response to determine if an
infection is from viral or bacterial etiology. In this presentation we
will focus on newer tests that have advanced point of care diagnostic
tests for common infections namely Group A streptococcal, influenza, and
RSV. The majority of tests currently for Group A strep, for example,
rely on detecting antigens in throat culture, but these lack sensitivity
(and specificity to some extent) and lead to significant number of false
negative results. This then leads to the need for back up laboratory
verification of point of care antigen tests, which in turn leads to
delays in correct prescribing, patient and clinical staff burden. New
point of care molecular tests for Group A strep offer very high
sensitivity and specificity, and are likely to replace existing rapid
antigen tests. Guidelines for Group A strep (as well as other common
infections such as influenza) are slowly shifting to acknowledge the
superior accuracy of point of care molecular tests.
This session will discuss the evidence of testing at the point of care
for influenza, RSV and Group A strep. It will also compare the
performance of different testing modalities, and discuss how diagnostics
can aid healthcare providers with their stewardship efforts.
This webinar will:
•
Discuss antimicrobial resistance and
antimicrobial prescribing patterns in the US, with a focus on acute
respiratory infections
•
Examine peer reviewed literature on the
performance of point of care diagnostic tests for influenza, RSV, and
Group A Strep
•
Review the benefits of decentralized testing
for respiratory pathogens
•
Analyze current guidelines and recommendations for detection of
respiratory pathogens
This session is sponsored by: |
 |
|
Presenter:
Matthew Thompson, MD, MPH, PhD
Professor, Dept Family Medicine, University of Washington, Seattle

Dr Thompson is the Helen D. Cohen endowed Professor and Vice Chair for
Research at the University of Washington Department of Family Medicine.
He completed his residency training in family medicine at the University
of Cincinnati, a Master’s degree in public health at the University of
Washington, and Doctorate at the University of Oxford. Dr Thompson has a
particular interest in improving the accuracy of diagnosis of
respiratory tract infections in order to guide more appropriate
antimicrobial prescribing. This research has included the use of point
of care tests for group A strep, influenza, and inflammatory markers. He
has also published extensively on the use of clinical prediction rules
to identify individuals at higher risk of serious infections. |
The Importance of Tissue Quality for Molecular Techniques
Live Event:
Thursday, September 5, 2019
|
1:00 - 2:00 PM EST
PACE®
credit available until March 5, 2020 | Florida Laboratory CE Credit
available |
 |
Invalid test results from next generation sequencing (NSG) and other
molecular assays negatively impacts patient care. The histology
laboratory supports molecular pathology through tissue specimen
preparation; and although we have learned over the last decade that
certain pre-analytical factors influence the outcome of
immunohistochemical assays, we are still learning what factors impact
molecular results.
In traditional histology we know that downstream methods cannot
compensate for a poorly fixed or processed tissue specimen. If a poor
quality tissue is processed, you will get a poor quality tissue out
again. Histology labs have created SOPs and techniques to help mitigate
this, and typically, routine surgical specimens deliver high quality H&E
slides and IHC slides. With the advent of molecular methods to detect
specific biomarkers, specimen quality definitions are evolving. What we
once treasured as a good quality tissue block for routine histopathology
and IHC may not necessarily meet quality standards for techniques such
as next generation sequencing or proteomics.
In this webinar we will consider what the requirements are for a high
quality specimen in the context of molecular methods, the technical
problems we sometimes encounter as histotechnologists while preparing
these specimens, and how we can mitigate these issues. Comparative
studies will be discussed, along with quality control methods to test
for tissue quality.
This webinar will:
•
Describe the tissue quality requirements for
optimal molecular pathology test results
•
Identify the steps required in the sample
preparation workflow for better results
•
Examine the quality control procedures
necessary in the histology lab to help ensure high quality specimen
This session is sponsored by: |
 |
|
Presenter:
Jennifer Freeland, MS, HTL(ASCP)cm
Global Market Development Manager, Epredia

Jennifer Freedland is a board of registry certified histotechnologist
with the American Society of Clinical Pathology. She has over 20 years
experience in routine histology, immunohistochemistry, and molecular and
cellular biology. She earned her Bachelors degree in Biomedical Science
from Western Michigan University and her Masters of Science degree in
Biotechnology from Johns Hopkins University. Jennifer has worked in
clinical histology and research labs, as well as research & development,
quality, technical consulting, and now serves as a global market
development manager for Epredia. |
New ASM C. Difficile Infection Guidelines and Rapid Diagnostic
Testing Recommendations
Live Event:
Thursday, August 29, 2019
|
1:00 - 2:00 PM EST
PACE®
credit available until February 29, 2020 | Florida Laboratory CE Credit
available |
 |
In a healthcare environment like a hospital or nursing home, Clostridium
difficile Infection (CDI) can be spread quickly through touching
contaminated surfaces or by person-to-person contact. C. difficile
causes an inflammation of the colon that can lead to serious,
life-threatening conditions, especially in immunocompromised or elderly
patients. The problem is so widespread, C. difficile infection (CDI) is
linked to more than 30,000 deaths a year in the United States — rivaling
the 32,000 killed in traffic accidents.
The demands for C. difficile testing have continued to evolve over the
last several years. While focus had been increasingly on the need for
highly accurate detection of the organism, there has been a renewed
interest in the detection of the toxins that cause the disease.
Colonized C. difficile carriers are 5-10 times more common than patients
with active infections in hospitals. Treating carriers is often
ineffective and increases the risk to the patient of developing C.
difficile diarrhea.
Increases in reported C.difficile infection (CDI) have spotlighted
diagnostic protocols and initiatives to reduce overcalling the disease.
This educational webinar provides expert perspectives on the recent
update to the ASM C.difficile infection guidelines and a review of IDSA
guidelines and other clinical evidence that describe the analytical and
clinical utility of diagnostic tests and protocols for C.difficile.
This webinar will:
•
Review and analyze the latest ASM C.
difficile guidelines
•
Discuss IDSA guidelines and how guidelines fit into
clinical diagnosis
•
Review analytical detection vs. clinical diagnosis.
•
Identify and describe the various C. difficile
diagnostic test methods including EIA, PCR and other molecular methods
This session is sponsored by: |
 |
|
Presenter:
James Snyder, Ph.D., Professor of Pathology and
Laboratory Medicine and Chief of Microbiology, University of Louisville
Hospital
Dr. Snyder serves as the American Society for Microbiology
Representative to the Association of Public Health Laboratories (APHL)
Working Group for Response to Bioterrorism and Emerging Infectious
Diseases. He is a Member of the American Society for Microbiology
Laboratory Practices Committee, serves as the coordinator of the
Sentinel Level Laboratory Protocols for Biothreat and Emerging
Infectious Diseases and is a Member of the American Society for
Microbiology Expert Panel for the development of Evidenced-Based
Laboratory Guidelines. |
New IDSA Influenza Guidelines and Their Impact on Rapid Testing
Live Event:
Wednesday, August 21, 2019
|
1:00 - 2:00 PM EST
PACE®
credit available until February 21, 2020 | Florida Laboratory CE Credit
available |
 |
This educational webinar provides expert perspectives on rapid influenza
testing, recent IDSA guidelines and the value of rapid molecular
testing. Lateral flow tests for influenza are widely utilized in
assessing patients with suspected influenza for their speed and
relatively inexpensive cost. Results are available in as few as 4 to 16
minutes to help quickly guide treatment decisions and care pathways. New
test standards implemented in 2018 require at least 80% sensitivity for
influenza tests, however, remain less sensitive than molecular tests.
New IDSA influenza guidelines encourage the use of molecular tests,
which help increase detection and guide more appropriate and timely use
of antivirals and antibiotics. Dr. Cameron Wolfe, Associate Professor of
Medicine: Division of Infectious Diseases & International Health at Duke
University Medical Center and co-author on the latest IDSA guidelines,
will present the new flu guidelines and rationale for using tests with
higher sensitivity for improved clinical and patient benefits.
As there are multiple molecular tests for influenza, the decision and
process for selecting a rapid molecular flu test can be a significant
task. Our program will provide an overview of the various rapid flu
tests including the similarities and differences of rapid molecular
technology for both high volume flu testing and decentralized/point of
care applications. Studies showing the value of rapid molecular testing
will also be reviewed.
Lastly, we will spotlight the recent experience of selecting and
implementing rapid molecular influenza testing across an entire
integrated health network; hospital lab, emergency department, urgent
care and physician offices. Dr. Joel Mortensen, Director, Diagnostic
Infectious Diseases Testing Laboratory, Department of Pathology and
Laboratory Medicine at Cincinnati Children’s, will share his experience
on the evaluation process, decision and the implementation best
practices and key learnings to help guide others that may be embarking
on a similar project.
This webinar will:
•
Identify and describe the latest IDSA
influenza guidelines
•
Discuss of the various influenza test
methods including EIA, PCR and other molecular methods
•
Review evidence supporting the value
of rapid molecular influenza testing
•
Discuss the recent evaluation and
implementation of rapid molecular influenza testing across an integrated
health network
This session is sponsored by: |
 |
|
Presenters:
 Dr.
Cameron Wolfe, MBBS (Hons), MPH, FIDSA, CPDM, A.Mus.A,
Associate Professor of Medicine Dr.
Cameron Wolfe, MBBS (Hons), MPH, FIDSA, CPDM, A.Mus.A,
Associate Professor of Medicine
Duke University Medical Center
Dr. Wolfe is the Chief Medical Director for Duke’s Emerging
Pathogens Unit, which focuses on preparedness in the event of
emerging biothreats, and serves as one of the core Transplant
Infectious Disease faculty. He was appointed to the IDSA
Influenza Guidelines national working group and co-authored the
2018 Influenza guideline update published in Clinical Infectious
Diseases. |
|
 Joel
E. Mortensen Ph.D., FAAM, HCLD Joel
E. Mortensen Ph.D., FAAM, HCLD
Director, Diagnostic Infectious Diseases Testing Laboratory,
Cincinnati Children’s Hospital Medical Center
Dr. Mortensen is a Professor of Pathology and Laboratory
Medicine for graduate, residency and fellowship teaching
programs and has collaborated with faculty and fellows on more
than 100 peer-reviewed publications, case studies and text
chapters. He holds numerous positions on national and
professional boards and has been an invited speaker to dozens of
national and regional scientific conferences and other
educational events. |
|
Diagnostics for Group B Strep: The Role of the Clinical
Microbiology Lab in Prenatal Screening
Live Event:
Thursday, July 18, 2019 |
12:00 - 1:00 PM EST
PACE®
credit available until January 18, 2020 | Florida Laboratory CE Credit
available |
 |
Group B Streptococcus (GBS) is a leading cause of neonatal sepsis and
meningitis. Prenatal screening of pregnant women has decreased the rate
of early-onset GBS disease in the United States. The incidence of
late-onset GBS disease has largely remained unchanged by current
screening practices. Clinical microbiology laboratories can impact the
care of GBS colonized women and GBS infected neonates.
GBS screening recommendations include culture of a vagino-rectal
specimen at 35 – 37 weeks gestation using an enriched culture-based
approach. Molecular assays are associated with higher sensitivity and
specificity, with faster time to results as compared to culture and can
significantly improve patient care.
This webinar will review the current recommendations for GBS detection
in pregnant patients, highlight the various methods available to
clinical microbiology laboratories, and will discuss the role molecular
methods can play in detection of GBS by the clinical microbiology
laboratory.
This webinar will:
•
Discuss the current recommendations for GBS screening to detect
colonization of pregnant patients
•
Identify the role of clinical microbiology laboratories in GBS screening
•
Examine the utility of molecular-based testing for detection of GBS
colonization
This session is sponsored by: |
 |
|
Presenter:
Gerald A. Capraro, PhD, D(ABMM)
Carolinas Pathology Group, Atrium Health
Charlotte, North Carolina
Dr. Capraro is the medical director of the Clinical Microbiology
laboratory for Atrium Health in Charlotte, NC. He earned his PhD in
Microbiology & Immunology from Wake Forest University and completed his
fellowship training at the University of Nebraska Medical Center. He is
Board certified in Medical and Public Health Microbiology. He is
actively involved in the American Society for Microbiology, the
Pan-American Society for Clinical Virology, and CLSI. |
What you’re Missing in your Respiratory Pathogen Detection
Live Event:
Monday, June 24, 2019 |
1:00 - 2:00 PM EST
PACE®
credit available until December 24, 2019 | Florida Laboratory CE Credit
available |
 |
Influenza and non-Influenza respiratory tract virus related infections
are one of the most common reasons reported for physician visits and
hospitalization globally. The economic burden associated with these
viral infections, within the United States, are upwards of $50 billion
annually. Concomitant or subsequent co-infections of the respiratory
tract by pneumonia causing pathogenic bacteria like Streptococcus
pneumoniae, Haemophilus influenzae, Moraxella catarrhalis and
Staphylococcus aureus are often observed in patients suffering from
these respiratory viral infections and contribute to significant
co-morbidity and mortality.
While the development of new panel-based syndromic molecular solutions
for pathogen detection has provided benefits to laboratories, some
challenges still exist including throughput scalability, reducing the
cost per sample, and flexibility of content. Overcoming these challenges
is necessary in order to cater to the ever-changing needs of those
ordering the tests.
Join us as we discuss the impact that real-time PCR testing can have on
respiratory pathogen detection in laboratories. Hear from presenters at
laboratories that have implemented these solutions, gained greater
insights into respiratory pathogen detection, and scaled the solution to
meet varying throughput requirements.
This webinar will:
•
Identify the limitations in current traditional
testing methods for respiratory infections
•
Describe the importance of simultaneously testing
multiple pathogen types in respiratory infections – including viral,
bacterial, and fungal
•
Examine new technology options to help test
multiple respiratory pathogens simultaneously
•
Discuss the considerations involved in
transitioning to these new technologies
|
Presenters:
 Vijay
Singh, Ph.D. Vijay
Singh, Ph.D.
Managing Principal Scientist
Molecular Diagnostics
HealthTrack Rx
Dr. Singh is the Managing Principal Scientist for Molecular
Diagnostics at HealthTrackRx in Denton Texas. He leads molecular
tests for pathogen targets on the qPCR nanofluidics platform. He
completed his PhD in Molecular Biology and his Post-Doctoral
training in Metabolic Engineering at the University of North
Texas. |
|
 David
R. Hillyard, MD David
R. Hillyard, MD
Medical Director, Molecular Infectious Diseases
ARUP Laboratories
Dr. Hillyard is a professor of pathology at the University of
Utah School of Medicine. He received his MD from the Columbia
University College of Physicians and Surgeons. His training was
in anatomic and clinical pathology, with fellowships in medical
microbiology and microbial genetics. |
|
Urine Drug Testing and its Impact on the Opioid Crisis
Live Event:
Tuesday, June 18, 2019 |
1:00 - 2:00 PM EST
PACE®
credit available until December 18, 2019 | Florida Laboratory CE Credit
available |
 |
There continues to be an opioid epidemic in the US with 2.4 million
Americans estimated to have an opioid disorder and over 42,000 dying
from drug overdose every year. Today clinicians are facing legal risk
regarding the opioid prescriptions that they are writing and if any
testing were done before and during the length of these prescriptions.
To help combat this opioid crisis the CDC, CMS and AACC have developed
testing guidelines for screening and monitoring.
The webinar will discuss the crisis, the current testing guidelines and
how best to screen and monitor patients that are prescribed opioids. We
will go through real life case studies in which testing had a positive
impact on patient care and offer suggestions on best practices for
implementing opioid testing protocols in your own facility.
This webinar will:
•
Differentiate between In-Office Qualitative Testing
& Laboratory Quantitative Testing
•
Discuss the legal risk of not screening and
monitoring for Opioids
•
Discuss methods used to interpret unexpected Urine
Drug Testing results
•
Explain how to incorporate Urine Drug Testing
results into ongoing clinical assessment and decision making
This session is sponsored by: |
 |
|
Presenter:
Jeffrey Fudin, B.S., Pharm.D., FCCP, FASHP,
Anesthesiology/Pain Management at Albany Medical Center Hospital
CEO and CMO, Remitigate, LLC, Delmar, NY
Dr. Fudin serves on the New York State Board of Medicine Office of
Professional Conduct. He is a Diplomate to the Academy of Integrative
Pain Management and a Fellow of both the American College of Clinical
Pharmacy and the American Society of Health-system Pharmacists. He is
considered a national expert in pharmacogenetics, forensic pharmacy, and
advanced pain therapeutics. |
Urinary Tract Infections: Improving Clinical Management and Outcomes
Live Event:
Wednesday, May 29,
2019 |
1:00 - 2:00 PM EST
PACE®
credit available until November 29, 2019 | Florida Laboratory CE Credit
available |
 |
There are
more than 250 million UTIs diagnosed worldwide each year, accounting for
$6 billion in direct healthcare expenditures, a 21% hospital readmission
rate in the US and a 2.3% mortality rate. Because the incidence and cost
to the healthcare system is so significant and urine samples are one of
the highest volume specimen types received in a clinical microbiology
laboratory, proper management of testing is critical to both the
laboratory workflow and to patient diagnosis and treatment. UTIs are not
only the most common human bacterial infection, they are also the most
common reason for prescribing antibiotics. By providing robust
diagnostic test results in a shorter timeframe, the level of unnecessary
administration of empiric antibiotics should be greatly reduced,
facilitating antibiotic stewardship and, ultimately, improving patient
care.
This webinar will provide an overview of these approaches and review
published studies comparing the new technologies to gold-standard
methods. It will also help participants understand the true economic
costs of UTIs and potential strategies to help reduce the work-flow
burden and costs in hospital laboratories.
This webinar will:
•
Review the burden
of
UTIs in dollars, time and health outcomes
•
Discuss available diagnostic technologies to detect
UTIs
•
Describe the correlation between rising antibiotic
resistance and inappropriate antibiotic treatments
•
Identify opportunities to improve clinical
management of UTI to improve patient care and outcomes
|
This session is sponsored by: |
 |
|
Presenter:
Rangaraj Selvarangan, BVSc, PhD,
D(ABMM), FIDSA, Professor
UMKC School of Medicine

Dr. Rangaraj Selvarangan is the Director of Microbiology and Virology
Laboratory and Director of Laboratory Medicine Research at Children’s
Mercy Hospital in Kansas City. He is a Professor in Department of
Pathology and Laboratory Medicine at University of Missouri-Kansas City
School of Medicine and Professor in Division of Infectious Diseases,
Children’s Mercy Hospital.
|
The Etiology of Community-Acquired Pneumonia:
Does Data Support the Guidelines?
Live Event:
Thursday, May 23,
2019 |
1:00 - 2:00 PM EST
PACE®
credit available until November 23, 2019 | Florida Laboratory CE Credit
available |
 |
Pneumonia is an acute alveolar lung infection that presents with
infiltrates upon chest imaging and is often accompanied by fever, cough,
sputum production, and physical findings of consolidation and elevated
white blood counts.1
Globally, pneumonia causes more deaths than any other infectious disease
and, along with influenza, is the eighth leading cause of death in the
United States.1,2
Community-acquired pneumonia (CAP) can be caused by bacterial, viral,
fungal, and zoonotic organisms and can cause mild to severe illness in
people of all ages. Certain people are more likely to become ill with
pneumonia. This includes adults 65 years of age or older and children
less than 5 years of age.2 Pneumonia can often be prevented with
vaccines and can usually be treated with antibiotics or antiviral drugs.
The diagnosis of CAP by clinical presentation along with the presence of
diagnostic chest x-ray findings can help guide empiric treatment with
the most narrow spectrum and safest drug possible. In this webinar,
we’ll review organisms currently thought to cause CAP, describe the
possible role of normal respiratory flora as an etiologic agent of CAP,
and relate guidelines for empiric therapy to the etiologic agents.
References:
1Woolfrey KG. Pneumonia in adults: the practical emergency
department perspective. Emerg Med Clin North Am. 2012; 30(2):249-70.
2http://www.who.int/mediacentre/factsheets/fs331/en/index.html
3https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_05.pdf
This webinar will:
•
Recognize organisms currently thought to cause
community-acquired pneumonia
•
Describe the possible role of normal respiratory
flora as an etiologic agent of CAP
•
Examine the relationship between guidelines for
empiric therapy and the etiologic agents
|
This session is sponsored by: |
 |
|
Presenter:
Daniel M. Musher, M.D.
Professor of Medicine-Infectious Disease
Baylor College of Medicine

Listed as one of the best doctors in the nation in the field of
infectious disease, Daniel M. Musher, M.D., Infectious Disease Section
chief at the Michael E. DeBakey VA Medical Center (MEDVAMC) and
professor of Medicine-Infectious Disease at Baylor College of Medicine,
is the recipient of the 2007 Infectious Diseases Society of America
Clinical Teacher Award from the Infectious Disease Society of America. A
national expert in respiratory and gastrointestinal infections, he is a
frequent author of review articles for prestigious medical journals such
as the New England Journal of Medicine. Dr. Musher holds a VA Merit
Review grant for study of immunization to protect veterans against
pneumococcal pneumonia. |
Next Generation Sequencing Implementation in a
Clinical Molecular Diagnostics Laboratory
Live Event:
Wednesday, May 1,
2019 |
1:00 - 2:00 PM EST
PACE®
credit available until November 1, 2019 | Florida Laboratory CE Credit
available |
 |
Next-generation sequencing (NGS) has quickly emerged as a useful tool to
study multiple genes and mutation types in a single assay, thus
preserving tissue and reducing time to results. Sentara Healthcare is a
regional hospital system spanning 12 hospitals and more than 200
physicians’ offices across Virginia and North Carolina. The molecular
diagnostics lab, located at its flagship hospital, serves as the
reference lab for the entire system. Through test menu optimization,
provider outreach, capital acquisitions and method validations, the
molecular diagnostics reference lab has been able to successfully
insource and implement NGS testing within the Sentara Healthcare
network.
Insourcing NGS has affected aspects of the lab such as tissue
conservation, turnaround times and costs. NGS implementation to
streamline genetic and molecular testing will be discussed throughout
this presentation. The webinar will describe how next generation
sequencing has emerged as a useful tool to study multiple genes and
mutation types in a single assay and illustrate how a molecular
diagnostics reference lab has successfully implemented NGS testing
within the Sentara Healthcare Network.
This webinar will:
•
Describe how next generation sequencing has emerged as a useful tool to
study multiple genes and mutation types in a single assay
•
Illustrate how a molecular diagnostics reference lab has
successfully implemented NGS testing within the Sentara Healthcare
Network
•
Discuss the ways in which this implementation has affected tissue
conservation, turnaround times and costs
|
Presenter:
Tabetha Sundin, PhD, HCLD (ABB), MB (ASCP)CM,
Scientific Director Molecular Diagnostics and Serology
Sentara Healthcare, Norfolk, VA

Tabetha Sundin, PhD, HCLD (ABB), MB (ASCP)CM, has over 10 years of
laboratory experience in cancer biology and clinical molecular
diagnostics. She is an active member of the Association of Molecular
Pathology (AMP) and involved with numerous efforts to support the
molecular diagnostics field with American Medical Technologists (AMT)
and Clinical & Laboratory Standards Institute (CLSI). |
Challenging Bacterial Infections:
The Clinical Impact of
Critical Microbiology Results
Live Event:
Tuesday, April 23, 2019 |
3:00 - 4:00 PM EST
PACE®
credit available until October 23, 2019 | Florida Laboratory CE Credit
available |
 |
Clinicians expect the microbiology laboratory to provide accurate
antimicrobial susceptibility testing results to guide their treatment
decisions. Reliable susceptibility results are never more important than
when addressing today’s most serious bacterial infections including
carbapenem-resistant Enterobacteriaceae, Pseudomonas and Acinetobacter.
By attending this webinar, microbiologists will learn how they can help
steer antibiotic treatment choices that are critical to patient care,
including reliable detection of existing and emerging resistance to new
drugs, as well as antimicrobials of last resort. Clinicians will have an
opportunity to gain insight into the results from microbiology
laboratories that can potentially impact patient care.
This webinar will:
•
Discuss a challenging case from a clinical and laboratory perspective
•
Evaluate testing options for rapid identification of resistant
infections
•
Discuss changing epidemiology of Candida infections
•
Discuss the need for ongoing breakpoint updates
|
This session is sponsored by: |
 |
|
Presenter:
James A. McKinnell, MD
Assistant Professor of Medicine
David Geffen School of Medicine, University of California, Los Angeles
James A. McKinnell, M.D. is an Assistant Professor of Medicine at the
David Geffen School of Medicine at the University of California, Los
Angeles. He is a nationally-recognized infectious disease specialist
with specific research interests related to the clinical management and
prevention of healthcare-associated infections. He has published over 40
papers, many with emphasis on optimal use of antibiotics and
antimicrobial resistance within the community. |
Biotin May Interfere with Lab Tests: The Impact is Coast to
Coast
Live Event:
Tuesday, February 5, 2019 |
1:00 - 2:00 PM EST
PACE®
credit available until August 5, 2019 | Florida Laboratory CE Credit
available |
 |
Market Research data shows that Biotin supplements continue to grow
based on their use for health and beauty. Retail stores continue to show
high levels of sales growth of Biotin doses of 10,000 mcg, not to
mention that Biotin currently is the #1 selling supplement on Amazon.
Biotin has been in the news due to the interference it can cause for
certain technologies that exists in the market place for laboratory
testing. With the high concentration of biotin that people are taking,
it is important to know the facts and options available when treating
patients. Our presenter will share firsthand stories illustrating the
science behind what causes the interference, how Biotin interference has
impacted the nation and how he has mitigated risk of potential
interference at his facility.
This webinar will:
•
Describe the magnitude of Biotin consumption in the U.S.
•
Illustrate the science behind how Biotin supplementation can potentially
impact lab test results through firsthand stories from an experienced
lab director
•
Examine methods to eliminate the risk of biotin interference in the
laboratory
|
Presenter:
Spencer Waitman, MLS, (ASCP)
Laboratory Director
Medical Park Family Care

Spencer Waitman MLS (ASCP) cm is currently the Laboratory Director at
Medical Family Care Inc. in Anchorage, Alaska. Spencer has over 15 years
of experience with Clinical Lab Medicine and continues to be a thought
leader when providing clinical decision support to his patients. |
H. pylori Diagnosis: Considerations for Selecting the
Appropriate
Testing Methodology
Live Event:
Wednesday, December 5, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until June 5, 2019 | Florida Laboratory CE Credit
available |
 |
In the United States, 20% of the population under 30 and 50% of the
population over 60 are infected with H. pylori. H. pylori
infections may be asymptomatic, but can lead to dyspepsia or serious
complications such as duodenal and gastric ulcers, an increased risk of
gastric cancer and higher rates of mucosal associated lymphoid-type
lymphoma.
Several invasive and non-invasive methodologies are currently available
for determining current infection, before and after eradication therapy.
Each testing methodology for H. pylori poses advantages and
disadvantages to the laboratory, patient, and institution. In this
webinar, we explore how to select the appropriate testing methodology by
balancing performance, economics, workflow, and patient care.
This webinar will:
•
Evaluate the appropriate testing methodology
by balancing performance, economics, and workflow
•
Discuss the best patient care by providing
accurate results for appropriate care within a test-treat-test
framework, while also taking into account economic and convenience
considerations for the patient
•
Examine the process of protecting the economic health and reputation of
the institution while providng the best patient care
|
Presenter:
David Lyerly, PhD
Chief Scientific Officer
TECHLAB

David Lyerly, Ph.D. has published >120 peer-reviewed publications on
intestinal disease. He is a frequent invited speaker at regional,
national, and international meetings and an invited reviewer for
numerous journals and committees. |
Implementing Next-Generation Sequencing for Precision Oncology
Testing
Live Event:
Thursday, November 29, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until May 29, 2019 | Florida Laboratory CE Credit
available |
 |
According to a recent study by the Tufts Center for the Study of Drug
Development, the majority of cancer treatments in the pipeline have an
associated genomic biomarker and this trend is expected to increase in
the coming years. With this evolution in the clinical oncology
landscape, academic medical centers and hospital systems alike have
adopted diagnostic precision medicine tools like next-generation
sequencing (NGS). NGS enables labs to rapidly and simultaneously test
many genomic biomarkers from just a few nanograms of precious
formalin-fixed paraffin-embedded (FFPE) clinical specimens. As the
number of clinically actionable biomarkers continues to expand, these
approaches will continue to play a critical diagnostic role in the
clinical laboratory setting.
In this webinar, our expert speaker will highlight the clinical and
economic considerations for implementing an NGS-based personalized
medicine program and discuss case studies that demonstrate the benefits
of broad genomic profiling across a wide variety of cancer types.
This webinar will:
•
Describe the decision making process in deciding whether to
implement next-generation sequencing in a clinical pathology lab setting
•
Identify the variety of testing strategies and chemistries
available
•
Review example case studies where NGS is uniquely suited to
provide novel clinical insights
|
Presenter:
Brian D. Piening, PhD
Associate Director, Providence St. Joseph Health (PSJH), Molecular
Genomics Laboratory

Dr. Piening is currently the Associate Director of the Providence St.
Joseph Health (PSJH) Molecular Genomics Laboratory and Assistant Member
and head of the Tumor Immunogenomics Laboratory at the Earle A. Chiles
Research Institute and Providence Cancer Center in Portland, OR. |
The Status of Microsatellite Instability Testing and its Role in
Colorectal Cancer
Live Event:
Monday, November 19, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until May 19, 2019 | Florida Laboratory CE Credit
available |
 |
Microsatellite Instability (MSI) is a hyper-mutation phenotype resulting
from mutations in one or more mismatch repair (MMR) proteins. MSI
testing has been a rapidly evolving field, both in terms of clinical
applications for MSI testing as well as methodologies available to
perform MSI testing. In the first portion of his talk, Dr. Mackinnon
will provide an update on the current state of MSI testing.
As requests for MSI evaluation increase, it will be important for labs
to be able to perform MSI testing in a timely and accurate manner.
Traditional molecular testing techniques for MSI are often challenging
to perform. They require high levels of operator expertise as well as
analysis of a normal tissue components, since the traditional biomarkers
are not tumor specific.
Dr. Mackinnon has evaluated a novel set of MSI biomarkers that are
analyzed by fully automated testing platform, making MSI testing
accessible to virtually any lab. He will present the performance data
from a cross-platform comparison of IHC and two different molecular MSI
evaluation methods and share results for 50 colorectal cancer samples
tested by all three methods.
This webinar will:
• Describe the two main testing
strategies for MSI testing
•
Identify the reasons/clinical applications
for performing MSI testing and what MSI-High vs. Microsatellite Stable
(MSS) results means
•
Analyze the performance of three MSI testing technologies, i.e., IHC + 2
molecular testing methods
|
Presenter:
Alexander Craig Mackinnon, MD PhD
Associate Professor of Pathology
Director, Clinical and Translational Research Core Lab
Dr. Mackinnon is an Associate Professor of Pathology and the current
Director of the Clinical and Translational Research Core Laboratory at
Medical College of Wisconsin in Milwaukee, WI. He received his
bachelor’s degree in biology from the University of Colorado and his
master’s degree in neuroscience from Northwestern University where he
spent time researching Alzheimer’s Disease. He went on to receive both
his MD and PhD in Cell and Structural Biology from the University of
Illinois at Urbana-Champaign. |
The Impact of Flexible Panel-Based Solutions for Pathogen
Detection
Live Event:
Wednesday, November 7, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until May 7, 2019 | Florida Laboratory CE Credit
available |
 |
The development of molecular testing methods for pathogen detection has
led to improved sensitivity, specificity and turnaround time compared
with traditional culture-based methods of analysis. However, current
commercially available molecular tests can be limited by the number of
set pathogenic markers. This means that if a result is not conclusive,
additional testing may be required – leading to increased time to
answer, and additional cost.
Panel-based, syndromic approaches to pathogen detection can present
numerous benefits to the clinical laboratory – including simplification
in ordering, testing of multiple pathogens above and beyond the “usual
suspects”, ease of use, rapid turnaround time, and reduced need to
send-out samples to other laboratories.
This webinar will provide you with the knowledge to understand the
economic and laboratory operational impact of using syndromic panels in
pathogen detection, and how this type of testing can be implemented in
the laboratory. Dr Schutzbank will lead a panel discussion of
laboratories from around the world that have implemented flexible
content syndromic testing for pathogen detection testing. To help
illustrate specific case studies in this area, Dr Sandeep Mukherjee will
then discuss the application of this in bacterial vaginitis
investigations, and Dr Li will discuss how this can impact respiratory
pathogen detection.
This webinar will:
•
Discuss the impact of flexible
content syndromic panels from a laboratory operational perspective
•
Describe how flexible content
syndromic panels affects the number of reflex tests the laboratory due
to test consolidation
•
Analyze the effects of flexible
content syndromic panels on laboratory costs
|
|
Presenters: |
|
 |
Ted E. Schutzbank PhD
Laboratory Dir., Quantigen Genomic Services |
|
|
|
 |
Kelly Li Ph.D.
Sr. Applications Scientist
Life Sciences Solutions
Thermo Fisher Scientific |
 |
Sandeep Mukherjee Ph.D.
Scientific Director
Women’s Health & Infectious Diseases
PathGroup |
|
100 Years Since the Spanish Flu: Current Standards for Flu
Pandemic Preparedness
Live Event:
Tuesday, October 16, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until April 16, 2019 | Florida Laboratory CE Credit
available |
  |
Last year’s influenza season was a challenging one with a recorded
higher prevalence of infection caused by what had been considered a less
virulent strain of the virus. This was compounded by a vaccine that did
not appear to be as effective against that particular strain along with
higher infant mortality and hospital admittance rates than had been
predicted. As a result of the higher prevalence of illness, there was a
shortage in the availability of rapid influenza tests which many clinics
and physicians experienced.
In this P.A.C.E.®-accredited Fisher Healthcare webinar, Dr.Sally Hojvat
will discuss the FDA's reclassification of rapid flu tests in detail.
She will also discuss how our understanding of the flu has advanced over
the past 100 years, and how we've been able to improve vaccination
strategies, surveillance, and our preparedness for future pandemics.
This webinar will:
•
Discuss the importance of having reliable, high performing diagnostic
tests, especially for higher risk patients
•
Describe how the FDA monitors compliance with the recently updated
performance standards for rapid flu tests
•
Explain how to determine whether a test meets FDA-required sensitivity
and specificity
•
Identify the most suitable tests for different testing scenarios
•
Review the pros and cons of molecular and
serological tests, plus manual and automated platforms
|
This session is sponsored by: |
 |
|
Presenter:
Sally Hojvat, PhD
Senior Consultant, Partners in Diagnostics

Dr. Sally Hojvat holds a PhD in Biochemistry from Loyola University,
before spending nearly two decades in the Diagnostic Division of Abbott
Laboratories. She then worked 12 years for the FDA as the Director of
the Division of Microbiology Devices and currently consults for the
World Health Organization (WHO) and other non-profit and commercial IVD
companies. |
Learn Lean: Simple Ways to Improve Lab Efficiency and Accuracy
Live Event:
Thursday, October 4, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until April 4, 2019 | Florida Laboratory CE Credit
available |
  |
Reimbursement for many tests is being reduced year by year, and the CMS
has stated that this will continue through 2020. Laboratories must
become more efficient. One way is to apply the proven Lean principles in
designing the way the work and the laboratory is structured.
Lean Manufacturing is based on principles that differ from the way
histology has been organized and practiced over the years. It is based
on small batches and limited inventory. The basics and the tools are
easy to learn, with a slight adjustment in the way we think about
organizing our work. By applying the thought process and some of the
tools, many laboratories have made significant advances in their
efficiency. It is quite possible to make a start with just the basic
training and some clear thinking.
This webinar is designed to provide that training. It will review and
redefine workflow in ways that will identify improvements, and identify
and implement ways of making workflow more efficient.
This webinar will:
•
Describe the basic principles underlying
Lean workflow planning
•
Identify and discuss the tools of Lean
Manufacturing
•
Apply these
principles to the laboratory to improve efficiency, reduce costs, and
reduce the risk of errors
|
Presenter:
Peter Kilner
Global Market Development Manager
Thermo Fisher Scientific

Peter Kilner is a Global Market Development Manager with Thermo Fisher
Scientific. He has previously held the posts of Marketing Manager in the
USA and in Europe, as well as Product Manager for tissue processing and
staining equipment. |
Liquid Based Microbiology:
Simplify Sample Collection and
Transport to Improve Patient Care
Live Event:
Wednesday, August 29, 2018 |
1:00 - 2:00 PM EDT
PACE®
credit available until February 28, 2019 | Florida Laboratory CE Credit
available |
 |
There are many challenges facing the clinical
microbiology laboratory today and tremendous pressure to perform quality
testing efficiently while limiting additional cost to the medical
institution. Many laboratories are being asked to streamline sample
collection
products due to consolidation. In doing so, laboratories must
strategically evaluate each sample to determine the best type of
collection and transport system.
SWABS
Traditionally, swab samples are collected using dacron or rayon swabs
which consist of yards of fiber wrapped around an applicator stick.
Using these swabs much of the patient sample becomes trapped in the
matrix of fiber. The result is that up to 90% of the sample stays with
the swab and is unavailable for testing. Fiber wrapped swabs are also
challenging to use on automated specimen processors without manual
intervention.
FECES
Currently, after collecting the fecal sample, a quantity (typically 1-2
grams) of feces is placed into a transport media tube. This process can
be unpleasant and messy. Traditional fecal containers are large and
bulky and not ideal for streamlined collection, transport or automation.
SPUTUM
Sputum is a challenging sample in the microbiology laboratory as it can
be very viscous and difficult to manage. To liquefy for easier manual or
automated specimen processing, liquefying solutions are often used.
These reagents are mixed in large batches which may go to waste if not
used within 48 hours.
URINE
Urine containers come in a variety of different shapes and sizes. The
vacuum style containers require the additional step of placing the
sample into a more automation friendly container/tube.
This webinar will give an overview of these approaches and review
published studies comparing the new technologies to gold-standard
methods.
This webinar will:
•
Identify the resources available to
validate, convert and train users on Liquid Based Microbiology (LBM)
products
•
Analyze clinical studies and impact of LBM
products on microbiology laboratories across the world
•
Discuss LBM
products and understand how they impact automation in clinical
microbiology
|
Presenter:
Susan Sharp, PhD., (D)ABMM, (F)AAM, MS, MT(ASCP)
Director of Scientific Affairs
Copan Diagnostics, Inc.

Dr. Sharp received her B.S. in Medical Technology and her M.S. in
Medical Microbiology & Biochemistry from the University of Nebraska
Medical Center in Omaha, Nebraska. She received her Ph.D. in Veterinary
Microbiology and Parasitology from the Veterinary School of Medicine,
Texas A&M University in College Station, Texas. She then did a 2-year
post-doctorate fellowship in Clinical Microbiology in the Department of
Pathology, Division of Microbiology, at Hartford Hospital in Hartford,
Connecticut.
|
Considerations in UTI Detection and its Potential Impact on
Antibiotic Stewardship
Live Event:
Tuesday, July 24, 2018 |
1:00 - 2:00 PM EDT
PACE®
credit available until January 23, 2018 | Florida Laboratory CE Credit
available |
  |
Urinary tract infections (UTI) are a leading cause of health care
visits. Consequently, urine specimens are one of the most frequent
specimen types submitted to laboratories, yet the majority of specimens
prove to be negative for UTI after evaluation by standard methods.
Plate-based culturing remains the gold standard for UTI detection,
requiring 24-48 hours before results are available. Urinalysis (UA) is
an automated approach that provides more rapid results than standard
culturing, but this method can suffer from poor sensitivity and
specificity, resulting in the improper management of patient care.
There are newer technologies available today that improve our ability to
detect UTI faster with higher specificity. These include mass
spectrometry and a newly approved technology that uses laser light
scatter to detect low density bacterial infection. By providing robust
results in a shorter timeframe, the level of unnecessary administration
of empiric antibiotics should be greatly reduced, facilitating
antibiotic stewardship and, ultimately, improving patient care. This
webinar will give an overview of these approaches and review published
studies comparing the new technologies to gold-standard methods.
This webinar will:
•
Describe the traditional and advanced diagnostic methods for UTI and
their impact on patient diagnosis.
•
Examine the role urinary tract infections play in inappropriate
antibiotic use and increasing antibiotic resistance.
•
Discuss the healthcare burden of UTIs in terms of dollars, time, and
health outcomes |
Presenter:
Erin H. Graf, Ph.D., D(ABMM), Director Infectious Disease Diagnostics
Laboratory
The Children's Hospital of Philadelphia

Dr. Graf is the Director of the Infectious Disease Diagnostics
Laboratory at the Children’s Hospital of Philadelphia. She is also an
Assistant Professor of Pathology and Laboratory Medicine at The
University of Pennsylvania. Dr. Graf completed her Ph.D. in Cell and
Molecular Biology in the Perelman School of Medicine at The University
of Pennsylvania studying HIV latency. Dr. Graf is board certified in
medical microbiology. Her research interests include sequence-based
diagnostics in clinical microbiology, including the applications of next
generation sequencing and metagenomics, as well as emerging technologies
for rapid diagnostics. |
Influenza Testing and the FDA Reclassification: Where do We Go
from Here?
Live Event:
Wednesday, June 6, 2018 |
1:00 - 2:00 PM EDT
PACE®
credit available until December 5, 2018 | Florida Laboratory CE Credit
available |
  |
FDA Influenza Reclassification went into full effect in January 2018.
This change placed additional requirements on influenza lateral flow
assay manufactures. As a result,, some assays were removed from the
market.
This change in influenza assay availability challenged some testing
facilities to adjust their assay use, or to purchase excess inventory
for the 2017/2018 influenza season. Now that the 2017/2018 influenza
season has passed, testing facilities that did not implement an
FDA-approved test will need determine their influenza testing plans for
the 2018/2019 influenza season and beyond.
This educational webinar will review flu testing challenges faced during
the 2017/2018 influenza season, including discussion on the management
and mitigation of highly seasonal testing and a review of testing
options for the 2018/2019 season. The session will also analyze the pros
and cons of each type of influenza testing.
This webinar will:
•
Review FDA Influenza Reclassification Requirements to provide
understanding of changes following the January 2018 enforcement date
•
Identify the different types of influenza tests available, following FDA
Influenza Reclassification
•
Analyze the pros and cons of each type of influenza testing
•
Discuss the 2017/2018 influenza season and lessons learned to prepare
for future season |
Presenter:
Gregory J. Berry, Ph.D., D(ABMM)
Director, Molecular Diagnostics
Assistant Director, Division of Infectious Disease Diagnostics
Northwell Health Laboratories

Dr. Berry is a Diplomate of the American Board of Medical
Microbiology and an Assistant Professor of Pathology and Laboratory
Medicine at the Donald and Barbara Zucker School of Medicine at
Hofstra/Northwell. He is also the Director of Molecular Diagnostics and
an Assistant Director of Infectious Disease Diagnostics at Northwell
Health Laboratories in New York. |
Reducing Time to Result for Urinary Tract Pathogen Detection
Utilizing Real-Time PCR Technology
Live Event:
Wednesday, May 30, 2018 |
1:00 - 2:00 PM EDT
PACE®
credit available until November 29, 2018 | Florida Laboratory CE Credit
available |
  |
Although widely used, culture-based methods for the detection of
pathogens involved in Urinary Tract Infections (UTI) can lack
sensitivity resulting in the possibility of pathogens not being
detected. They can also be subjective leading to misinterpretation of
results, take a long time resulting in reduced lab efficiency, and they
have been shown to miss a significant percentage of positive cases. In
fact, some studies show that almost 30% of positive cases are missed
using culture-based methods
A molecular alternative to culture-based methods, real-time PCR
technology, increases specificity and sensitivity, with over 25%
increased accuracy in urinary tract pathogen detection when compared to
culture methods in under 5 hours. Real-time PCR in pathogen detection
can identify slow-growing, difficult-to-cultivate microorganisms, and
can be used when culture-based techniques are inadequate, ambiguous,
time-consuming, difficult, and/or too costly. Clinical validation data
demonstrated that when compared with urine specimen culture, real-time
PCR detected 97% of samples where urinary tract pathogens were present,
vs culture which detected only 71% of cases where pathogens were
present.1
This webinar will compare molecular testing for urinary tract pathogen
detection to traditional culture-based testing methods, examine the
sensitivity, specificity and turnaround time of molecular testing
techniques for UTI pathogen detection, and discuss the current impact of
UTI’s in the US and globally, including health economic impacts and how
new testing methods can potentially impact laboratory efficiency.
1For research use only.
Not for use in diagnostic procedures.
This webinar will:
•
Compare molecular testing for urinary tract pathogen detection to
traditional culture-based testing methods
•
Examine the sensitivity, specificity and
turnaround time of molecular testing techniques for UTI pathogen
detection
•
Discuss the current impact of UTI’s in the
US and globally, including health economic impacts and how new testing
methods can potentially impact laboratory efficiency |
Presenter:
David Baunoch, PhD
President and Chief Executive Officer Pathnostics
 : :
With over 25 years of laboratory experience,
Dr. Baunoch has extensive experience in all areas of Lab Services. Dr.
Baunoch received his PhD in Microbiology and Molecular Genetics from
Wayne State University and completed a NIH Postdoctoral Fellowship in
Breast Cancer Research at the Michigan Cancer Foundation. He is widely
published, with over 25 peer-reviewed publications.
|
Clostridium difficile Infection Guideline Update:
Understanding the Data Behind the Recommendations
Live Event:
Tuesday, May 8, 2018 |
1:00 - 2:00 PM EDT
PACE®
credit available until November 7, 2018 | Florida Laboratory CE Credit
available |
  |
In a healthcare environment like a hospital or nursing home,
Clostridium difficile Infection (CDI) can be spread quickly through
touching contaminated surfaces or by person-to-person contact. C.
difficile causes an inflammation of the colon that can lead to
serious, life-threatening conditions, especially in immunocompromised or
elderly patients. The problem is so widespread, C. difficile
infection (CDI) is linked to more than 30,000 deaths a year in the
United States — rivaling the 32,000 killed in traffic accidents.
The demands for C. difficile testing have continued to evolve
over the last several years. While the focus had been increasingly on
the need for highly accurate detection of the organism, there has been a
renewed interest in the detection of the toxins that cause the disease.
Colonized C. difficile carriers are 5-10 times more common than
patients with active infections in hospitals. Treating carriers is often
ineffective and increases the risk to the patient of developing C.
difficile diarrhea.
C. difficile infections pose a serious threat and require rapid
clinical decisions. This webinar will review the 2017 IDSA/SHEA CDI
guideline update treatment recommendations, describe how the 2017
IDSA/SHEA CDI guideline update recommendations on C. difficile
diagnostics will apply to a patient population, and identify how the
microbiology laboratory can assist in C. difficile infection
prevention.
This webinar will:
•
Review the 2017 IDSA/SHEA CDI guideline
update treatment recommendations
•
Describe how the 2017 IDSA/SHEA CDI
guideline update recommendations on C. difficile diagnostics
will apply to a patient population
•
Identify how
the microbiology laboratory can assist in C. difficile
infection prevention
|
Presenter:
Erik Dubberke, MD
Associate Professor of Medicine
Washington University School of Medicine
St. Louis, MO

Dr. Dubberke is an Associate Professor of Medicine at Washington
University School of Medicine in St. Louis, where he has been a faculty
member in the Division of Infectious Diseases since 2005. His main
research interests are in the epidemiology, diagnosis, treatment, and
prevention of Clostridium difficile infection (CDI). He is the
lead author of the CDI component of the SHEA compendium to prevent
healthcare associated infections, and is a panel member on the update of
the SHEA/IDSA CDI clinical guidelines. |
Anti-Heparin Platelet Factor 4 Antibodies: Risking a Potentially
Catastrophic Occurrence
Live Event:
Thursday, April 5, 2018 |
1:00 - 2:00 PM EDT
PACE®
credit available until October 4, 2018 | Florida Laboratory CE Credit
available |
  |
As many as 5% of patients treated with heparin have an immune complex
that is formed between Heparin and Platelet Factor 4 (PF4). These
patients may develop Heparin Induced Thrombocytopenia (HIT),
characterized by a low platelet count that can result in excessive
bleeding or clotting. Of those diagnosed with HIT, 30% are at risk for
death and 20% are at risk for limb amputation.
Current testing for HIT can take several hours to several days for the
results. During this time, patients requiring surgery must wait for the
test results to determine if heparin can be administered, or they are
given expensive direct thrombin inhibitors (DTI’s) as a precautionary
measure.
This webinar will describe the mechanism of interaction between heparin
and platelet factor 4, review the chemistry of heparin, and identify the
consequences of antibodies to Heparin Platelet Factor 4. It will also
examine the testing methodology for the anti-Platelet Factor 4 Heparin
antibody.
This
webinar will:
•
Describe the mechanism of interaction between Heparin and
Platelet Factor 4
•
Review the chemistry of Heparin
•
Identify the consequences of antibodies to the Heparin Platelet
Factor 4
•
Examine the testing methodology for the anti-Platelet Factor 4
Heparin anti-body
|
This webinar is sponsored by |
 |
|
|
Presenter:
Michael Warhol, MD
Past President , Pennsylvania Association of Pathologists
Fellow of the American College of Pathology

Dr. Warhol received his undergraduate degree at Princeton University and
his M.D. degree from the University of Pittsburgh. He continued his
residency training in pathology at the Peter Bent Brigham Hospital,
Boston, MA. He served as Chairman and Director of Laboratories at
Pennsylvania Hospital in Philadelphia, PA and New York Hospital Queens. |
Empowering STAT DNA Testing for Molecular Oncology Applications using a
Fully Automated Platform
Live Event:
Thursday, March 15, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until September 14, 2018 | Florida Laboratory CE Credit
available |
  |
Turnaround time remains a major issue in molecular biomarker testing.
Current technologies are complex, require a lot of hands-on time and are
often difficult to implement in the local laboratory. These factors
significantly extend the time until the result report becomes available.
This webinar will provide firsthand perspectives about how new
technologies can help improve turnaround times in virtually any lab. Dr.
Tsongalis will discuss his experiences with fully -automated molecular
biomarker analysis by presenting results from a recent performance
study. He will also share his views on validation requirements for such
a platform.
This webinar will:
•
Discuss the reasons for the need for improvement
in TAT when it comes to testing Oncology biomarkers.
•
Compare the performance of a fully-automated
qPCR-based system to that of a Next-Generation Sequencing based system
•
Identify validation strategies for implementing
fully automated biomarker-testing systems in a CLIA setting.
|
Presenter:
Gregory J. Tsongalis, PhD, HCLD, CC
Professor of Pathology
Dartmouth Hitchcock Medical Center
Lebanon, NH

Dr. Tsongalis' research interests are in
the pathogenesis of solid tumors, disease association of SNP genotyping
and personalized medicine. He has authored/edited 11 textbooks in the
field of molecular pathology, published more than 200 peer reviewed
manuscripts, and has been an invited speaker at both national and
international meetings.
|
Understanding Community-Acquired Pneumonia and Treatment Options
Live Event:
Tuesday, January 9, 2018 |
1:00 - 2:00 PM EST
PACE®
credit available until July 8, 2018 | Florida Laboratory CE Credit
available |
  |
For patients with community-acquired pneumonia (CAP), the current
standard of practice is to start initial empiric antimicrobial therapy
using broad-spectrum antibiotics with the goal to cover the most likely
etiologies. Since the initial standard microbiological work-up fails to
identify a definitive etiology in the majority of patients, most
patients are continued on broad-spectrum antibiotics for the full
duration of therapy. This empiric current antimicrobial approach exposes
patients to more antimicrobials than necessary, eradicates a significant
proportion of organisms belonging to the normal host flora (collateral
damage), and selects for antimicrobial resistant pathogens.
However, with advances of diagnostic tests (including
immunochromatographic-based urinary antigen and molecular assays) which
can identify respiratory pathogens of CAP earlier in the course of
management and with the potential for identifying specific pathogens in
a greater proportion of patients, it is now possible to provide early
treatment with a narrower, focused antimicrobial regimen that targets
the identified pathogens. In those who have been begun on broader
coverage, antibiotics can be reduced or “de-escalated.” This
pathogen-directed therapy will ultimately lead to a new paradigm of
“targeted antimicrobial” treatment that will permit selection of agents
against a specific pathogen and substantially reduce exposure of
individuals and hospitals to antimicrobial agents with decreased
selection of antimicrobial resistance, cost, and adverse events.
This webinar will:
•
List the differences between empirical and
pathogen-directed therapy for community-acquired pneumonia
•
Review pathogens responsible for
community-acquired pneumonia
•
Analyze the diagnostics and treatment
options available for community-acquired pneumonia
•
Identify advantages of rapid diagnostic methods for community-acquired
pneumonia
|
Presenter:
Thomas M. File, Jr., MD MSc. MACP FIDSA FCCP
Chief of the Infectious Disease Service
Summa Health System, Akron, Ohio
Thomas M. File Jr., MD is Chief of the Infectious Disease Service and
Director of HIV Research at Summa Health System in Akron. Ohio, and
Professor of Internal Medicine and Master Teacher at the Northeastern
Ohio Universities College of Medicine in Rootstown, Ohio. |
Using Modern Technology to Surveil, Monitor, and Diagnose
Infectious Disease
Live Event:
Monday, December 18, 2017 |
1:00 - 2:00 PM EST
PACE® credit available
until June 18, 2018 | Florida Laboratory CE Credit
available |
  |
There is a growing need for accurate and timely information about the
status of infectious disease in a community, county or state. Such
information will alert physicians, hospital administrators, medical and
laboratory directors, and public health agencies, and can enable
preventive measures and/or improved patient care and management. Modern
surveillance technology shows great promise in fulfilling this need by
sending results in near real-time for influenza, RSV, and Strep A tests
to the CDC, state departments of health, and healthcare organizations
nation-wide.
This webinar will discuss recent technological advances that have
afforded certain FDA-cleared rapid point of care instruments that aid in
the diagnosis of infectious disease the capability to wirelessly convey
near real-time results and transmit to public health agencies and
organizations for use in de-identified surveillance and laboratory
management. The utility for laboratory management, featuring quality
control, training, resource management, and operator performance will be
discussed, as will the impact of valid real-time data on the management
of patients and the timely and appropriate use of antivirals and
antibiotics. Promising new applications of data in developing enhanced
disease forecasting and the benefits this promises for public health,
healthcare systems, pharmacies and others will be also be considered.
This webinar will:
•
Identify technology that allows certain FDA-cleared, rapid-POC testing
instruments to wirelessly transmit to public authorities
•
Describe how labs can use the technology for quality control, training
and resource management
•
Analyze the impact of valid real-time data on patient care management,
including the use of antivirals and antibiotics
•
Discuss promising new applications of data to enhance disease
forecasting and its benefits for various stakeholders
|
Presenter:
John Tamerius, PhD
Sr. Vice President, Strategic and External Affairs, Quidel Corp.

Dr. John Tamerius graduated from the Univ. of Washington (Seattle,
Washington) with a Ph.D. in Microbiology and Immunology. He performed
graduate and postdoctoral research in tumor immunology at the Fred
Hutchinson Cancer Center (Seattle) before joining the Scripps Clinic and
Research Foundation (San Diego, California) as a Research Associate in
the Dept. of Molecular Immunology. |
Meeting the Standards:
Mandatory FDA Reclassification Of Rapid Influenza Detection Tests
Live Event:
Monday, November 6, 2017 |
1:00 - 2:00 PM EST
PACE® credit available
until May 6, 2018 | Florida Laboratory CE Credit
available |
  |
FDA Tightens Standards, Reclassifies RIDTs
There have historically been some challenges with rapid immunoassay
detection test (RIDTs) for influenza and their variability in
performance. While they tend to show good specificity, they can deliver
less-than-optimal sensitivity in respiratory specimens compared to
RT-PCR or viral culture.
In some cases (for example, the H1N1 flu strain in 2009) RIDTs may be
unable to detect the virus at all. For this reason, negative RIDT test
results should be interpreted with caution given the potential for false
negative results - especially during peak flu season in a community.
Based on these concerns, the FDA began work to reclassify antigen-based
RIDTs as Class II devices in order to improve the overall quality of
testing for influenza. The FDA has provided certain performance criteria
that manufacturers will have to meet in order to market their influenza
assays.
What Does the FDA Reclassification Mean for RIDT Manufacturers?
Manufacturers must obtain a new 510(k) clearance and demonstrate
compliance with the special controls included in the new clinical
performance standards before marketing antigen-based RIDTs.
What Does the FDA Reclass Mean for Physicians and Labs?
Facilities testing for flu can still continue to purchase their current
product up until January 12, 2018 and utilize them until the kit’s
expiration date. This provides facilities enough time to assess the
performance data against the FDA criteria and engage clinicians and
management on the next course of action for flu testing.
This webinar will:
•
Describe the FDA reclassification of rapid
immunoassay detection tests (RIDT’s) for 2018
•
Discuss the reason for FDA’s implementation
of the new reclassification and how that impacts not only manufacturers
but also the physician, the laboratory, and the patient
•
Identify the information RIDT users must have from manufacturers to
determine whether or not their current testing meets the
reclassification |
Presenter:
Sally Hojvat, PhD

Sally Hojvat holds an MSc in Microbiology/ Food Science from the
University of Alberta and a PhD in Biochemistry from Loyola University.
She has completed post-doctorate work in clinical chemistry and
pharmacology, worked for the FDA, and has extensive experience working
for a major international IVD manufacturer.
|
Get the Most Out Of Barcoding In Your Pathology Laboratory
Live Event:
Wednesday, October 25, 2017 |
1:00 - 2:00 PM EST
PACE® credit available
until April 25, 2018 | Florida Laboratory CE Credit
available |
  |
Barcoding is used everywhere in our culture today to prevent errors. In
laboratories, barcoding has become an evidence based “best practice” for
reducing errors and improving productivity where up to 70% of all errors
occur in the pre- and post-analytic phases. Besides improving
productivity, barcoding opens up many new opportunities to utilize the
embedded data downstream through multiple stages up to and including
long-term storage and archiving.
This webinar will offer a practical approach to implementing a barcoding
solution to meet the needs of your individual laboratory for protecting
the integrity of patients’ specimens. With US Healthcare moving from a
Fee-for-Service model to a Value-Based system, laboratories must
implement ways of improving quality outcomes. The additional benefit
barcoding delivers is an improvement in productivity and reduction, to
the point of elimination of non-value added tasks. Barcoding utilized
along with lean processes has also been proven to reduce labeling errors
to near zero in pathology laboratories.
This webinar will:
•
Describe how reimbursement impacts technology utilization in
the laboratory
•
Differentiate between linear and 2D barcodes and how each
captures patient data
•
Review techniques labs employ to adapt barcoding to their
varying sizes and budgets
•
Illustrate the ways in which barcoding affects a pathology
laboratory's workflow and productivity
|
Presenter:
Loretta Sayles
Sayles Lab Consulting

Loretta Sayles has spent the past 30 plus years working in the anatomic
pathology laboratory arena in several different aspects of our business.
She currently is the Managing Director of Sayles Lab Consulting which
focuses on helping labs improve their quality while understanding the
challenging healthcare market. Loretta is very active in Histotechnology
on both the national and state level and has been recognized for her
dedication to the field. |
The Journey to Realizing the Promise of Precision Medicine
Live Event:
Tuesday, October 17, 2017 |
1:00 - 2:00 PM EST
PACE® credit available
until April 17, 2018 | Florida Laboratory CE Credit
available |
 |
Currently, clinical labs are doing
sequential, single-analyte testing in oncology which exhausts precious
patient samples and extends the turnaround time to results. Clinicians
can wait for as long as two to three weeks to get a result. And, if the
sample is insufficient for molecular testing, patients can be subject to
expensive and painful rebiopsies. Pathologists and other clinicians need
a better, faster way to consolidate their molecular testing into a
single assay and get results within a week.
This webinar will show how Next-Generation Sequencing (NGS) is helping
labs save precious samples and provide rapid results. It will review the
updates on the NCI-MATCH clinical trial for adult cancers and the
development of a gene panel specific to pediatric cancers, and it will
discuss a laboratory's implementation of next-generation sequencing for
cancer clinical research.
This webinar will:
•
Review the updates on the NCI-MATCH clinical
trial for adult cancers and the development of a gene panel specific to
pediatric cancers
•
Analyze the effects of next-generation
sequencing on the speed of results from the clinical/pathology lab to
oncologists to minimize the need for a painful and expensive rebiopsy
•
Discuss a laboratory's implementation of
next-generation sequencing for cancer clinical research
|
| Presenters: |
 Timothy
Triche, MD, PhD, Pathologist; Co-Director, Center for
Personalized Medicine Program (CPM) Professor of Pathology and
Pediatrics, USC Keck School of Medicine Timothy
Triche, MD, PhD, Pathologist; Co-Director, Center for
Personalized Medicine Program (CPM) Professor of Pathology and
Pediatrics, USC Keck School of Medicine |
|
 Mickey
Williams, PhD Mickey
Williams, PhD
Director, Molecular Characterization Laboratory, National Cancer
Institute |
|
 Barbara
A. Conley, MD Special Volunteer / Contractor, National
Cancer Institute Barbara
A. Conley, MD Special Volunteer / Contractor, National
Cancer Institute |
|
HIV Trends, Guideline Recommendations, & the Evolution of Rapid HIV
Screening Tests
Live Event:
Thursday, September 28, 2017 |
1:00 - 2:00 PM EST
PACE® credit available
until March 28, 2018 | Florida Laboratory CE Credit
available |
  |
The Center for Disease Control (CDC)
estimates that 14 percent of people infected with HIV in the United
States - more than 168,000 people1 - are unaware of their
infection. Of the estimated 50,000 new
HIV infections each year, thousands are transmitted by people who do not
know that they are HIV-positive.2,3
With the successful introduction of antiviral drugs, HIV screening and
testing has become a cornerstone for prevention and treatment. For those
who test positive, it opens the door to life-saving treatment and
reduces the transmission of HIV to others. And for those who test
negative, they can take preventative measures to ensure they remain
negative.
Through the years, HIV screening tests have improved in performance and
ease of use but not all HIV tests are equal. The CDC in 2014 updated
their recommendations on HIV testing to include screening with a 4th
generation lab test. This webinar will review the evolution of HIV
screening tests, identify differences in HIV testing methodologies,
review current CDC and HRSA guidelines for HIV testing, screening, and
analysis, and develop strategies within one’s own institution to
increase screening for HIV.
1
CDC. Monitoring selected national HIV prevention and care objectives by
using HIV surveillance data - United States and 6 U.S. dependent areas -
2012. HIV Surveillance Supplemental Report 2014;19(No. 3). Available at:
http://www.cdc.gov/hiv/library/reports. Published November 2014.
(Accessed November 25, 2014).
2 CDC. Estimated HIV incidence among adults and adolescents
in the United States, 2007-2010. HIV Surveillance Supplemental Report
2012;17(No. 4). Available at:
http://www.cdc.gov/hiv/topics/surveillance/resources/reports/ttsupplemental.
Published December 2012.
3 Hall HI, Holtgrave DR, and Maulsby C. HIV transmission
rates from persons living with HIV who are aware and unaware of their
infection. AIDS 2012;26(7):893-96.
This webinar will:
•
Review current CDC and HRSA guidelines for HIV
testing/screening/analysis and importance of early detection
•
Determine the patient population that can benefit from
rapid point-of-care testing for HIV antigen/antibody
•
Develop strategies within one’s own institution to
increase screening for HIV
•
Apply current guidelines and best practices to improve
the care of patients who are HIV positive and HIV negative |
Presenter:
Neil W. Anderson, MD
Assistant Professor, Washington University School of Medicine, and
Asst Medical Dir, Clinical Microbiology,
Barnes Jewish Hospital
St. Louis, Missouri

Neil Anderson completed his training in anatomic and clinical pathology
at the Medical College of Wisconsin, followed by a fellowship in
clinical microbiology at Mayo Clinic. He currently is an assistant
professor at Washington University in Saint Louis School of Medicine and
is the assistant medical director of clinical microbiology at Barnes
Jewish Hospital. His areas of academic pursuit include the serologic and
molecular testing for infectious diseases, with a particular focus on
HIV testing. |
Advances in Biomarker Testing for Sepsis and Bacterial
Infections
Live Event:
Wednesday, September 13, 2017 |
1:00 - 2:00 PM EST
PACE® credit available
until March 13, 2018 | Florida Laboratory CE Credit
available |
  |
|
Systemic bacterial Infections are often difficult to differentiate
from other infections. This can lead to a delay in appropriate treatment
and sometimes overtreatment with antibiotics Both the clinical
presentation and diagnostic tests are required to manage therapy.
Timely, informed decisions can be made with the assistance of
biomarkers. With the recently FDA approved claim extensions of
Procalcitonin (PCT) clinicians now have an additional tool to help
direct antibiotic therapy. This can result in reduced antibiotic usage,
reduced time in ICU reducing the costs incurred by both patients and
healthcare systems while improving clinical outcomes.
This webinar will provide a thorough understanding on how biomarkers are
used in systemic bacterial infections and Lower Respiratory Tract
Infections (LRTI) and the laboratory’s role in helping direct patient
therapy. It will analyze PCT as an infection biomarker with a review of
the recently approved FDA claims and discuss the clinical application of
the biomarker using case studies for LRTI and Sepsis.
This webinar will::
•
Identify the various biomarkers used to assess
systemic infections
•
Discuss PCT as an infection biomarker with a
review of the recently approved FDA claims
•
Define the role of PCT in the context of
antibiotic stewardship
•
Describe the clinical application of the
biomarker using case studies for LRTI and Sepsis
|
Presenter:
Eric Gluck MD, FCCP JD
Director, Critical Care Services
Swedish Covenant Hospital
Chicago, Illinois

Dr. Gluck is a Professor of Medicine at Finch University of Health
Sciences/The Chicago Medical School in North Chicago. He has previously
held positions as an Assistant Professor at both Rush-Presbyterian St.
Luke’s Medical Center and the University of Connecticut. Dr. Gluck is
Board Certified in Internal Medicine with subspecialties in Pulmonary
and Critical Care Medicine. |
Genital Zoster Infections: An Unexpected Finding Using a Molecular Assay
Live Event:
Thursday, July 27, 2017 |
1:00 - 2:00 PM EST
PACE® credit available
until January 27, 2018 | Florida Laboratory CE Credit
available |
  |
Herpes simplex virus (HSV) and Varicella-zoster virus (VZV) are common
causes of cutaneous and mucocutaneous infections and typically
distinguished based upon appearance and anatomic location. But atypical
presentations of zoster can occur in unusual anatomical sites. Improved
testing methods for the differentiation of HSV 1+2 and VZV from
cutaneous and mucocutaneous specimens allow for correct detection and
diagnosis leading to better treatment and patient counseling.
Incorrect diagnosis of suspected HSV has psychosocial impacts that
affect patient well being. Traditional culture methods for HSV and VZV
can take between 24 hours and 2 weeks for results which can delay
therapy and leave patients in the dark.
Molecular testing methods to diagnose and differentiate Herpes from
Varicella Zoster can change treatment and patient counseling by
providing definitive results in a timely manner to allow for more
accurate treatment.
This webinar will:
•
Discuss the importance of differentiating HSV
from VZV specifically in genital lesions
•
Examine the ways in which a fast TAT for VZV can
impact clinical care
•
Analyze the psychosocial impact of an incorrect
diagnosis for HSV/VZV
•
Identify the treatment differences and positivity
rates for VZV in patients suspected to have HSV
|
This webinar is sponsored by |
 |
and |
 |
|
Presenter:
Paul A. Granato, Ph.D., DABMM, FAAM
Professor Emeritus of Pathology
SUNY Upstate Medical University

Dr. Granato earned his Ph.D. in microbiology and molecular biology from
Syracuse University after graduating from Le Moyne College majoring in
biology and chemistry. Dr. Granato directed several clinical
microbiology laboratories over his professional career while serving as
a faculty member in the Departments of Pathology and Microbiology &
Immunology at SUNY Upstate Medical University for over 35 years where he
is now Professor Emeritus in Pathology.
|
Differentiating Gluten-Related Disorders Through Diagnostic
Methods
Live Event:
Monday, June 19, 2017 |
2:00 - 3:00 PM EST
PACE® credit available
until December 19, 2017 | Florida Laboratory CE Credit
available |
  |
Celiac Disease is an immune-mediated systemic disorder elicited by
gluten and related prolamines in genetically susceptible individuals.
Approximately 90% of CD patients are not yet diagnosed. 36% of CD
patients are incorrectly diagnosed with irritable bowel syndrome. The
incidence of CD has increased from 5.2 per 100,000 persons in 1990 to
19.1 in 2010. Differentiation is critical since a gluten restricted diet
is a burden for the patient and family.
Wheat is a grass, and one of the most common causes of food allergen
sensitization in children. Some grass sensitized children can be
misdiagnosed as wheat allergic who are recommended a wheat-free diet as
whole wheat extract tests often show sensitization due to
cross-reactivity between wheat and grass components e.g. profilin and
CCD. Wheat is an ingredient in processed foods other than bakery
products, for instance in beer which may elicit symptoms in allergen
sensitized patients.
This session will present an update of our current understanding of the
three main forms of reactions to wheat and its byproducts including
gluten: allergic (wheat allergy), autoimmune (celiac disease) and
intolerance (gluten sensitivity). The speakers cover testing cascades to
differentiate patients efficiently, as well as the laboratory efficiency
gains by processing these tests on a single automated platform.
This webinar will:
•
Discuss the prevalence, symptoms, and characteristics of
three "gluten"- related disorders
•
Examine the reasons why "Non-celiac Gluten Sensitivity (NCGS)" is
still a vague umbrella term encompassing distinct populations of
patients
•
Identify the patients who would benefit from testing
•
Assess specific testing cascades to assist the clinician in the
differentiation between "gluten"- related disorders |
Presenters:
 Stefano Guandalini, MD, is an internationally recognized expert on
celiac disease. He is also known for
his expertise in the research and treatment of other diarrheal diseases
in children. Dr. Guandalini is the president of the North American
Society for the Study of Celiac Disease, and has been ranked among
America’s "Best Doctors" since 2008. Stefano Guandalini, MD, is an internationally recognized expert on
celiac disease. He is also known for
his expertise in the research and treatment of other diarrheal diseases
in children. Dr. Guandalini is the president of the North American
Society for the Study of Celiac Disease, and has been ranked among
America’s "Best Doctors" since 2008. |
|
 Dr.
Alessio Fasano is chief of pediatric gastroenterology
and nutrition at Mass General Hospital for Children (MGHfC). He
is a world-renowned pediatric gastro-enterologist, research
scientist and entrepreneur. Dr. Fasano directs the Center for
Celiac Research, specializing in the treatment of patients of
all ages with gluten-related disorders, including celiac
disease, wheat allergy and gluten sensitivity. Dr.
Alessio Fasano is chief of pediatric gastroenterology
and nutrition at Mass General Hospital for Children (MGHfC). He
is a world-renowned pediatric gastro-enterologist, research
scientist and entrepreneur. Dr. Fasano directs the Center for
Celiac Research, specializing in the treatment of patients of
all ages with gluten-related disorders, including celiac
disease, wheat allergy and gluten sensitivity. |
|
Vaginal Microbiota Investigations: Increasing Insight, Reducing Cost
Live Event: Tuesday, May 16, 2017 |
2:00 - 3:00 PM EST
PACE® credit available
until November 16, 2017 | Florida Laboratory CE Credit
available |
  |
|
Urogenital infections,
including bacterial vaginosis, urinary tract infections, and vaginitis,
afflict over a billion women each year. In spite of the significant size
of the affected population, there is a lack of awareness among CLIA labs
for a multi-pathogen solution for screening vaginal microbiota. Current
culture based methods for vaginal and urogenital microbiota lack
sensitivity and specificity, and are subjective as well as inaccurate.
Current molecular methods for bacterial vaginitis can have a high cost
per sample, lack of flexibility in content and pathogenic targets, and
are not amenable to centralized testing. Tests that are neither flexible
in content, low cost per sample, nor sensitive enough to detect vaginal
and urogenital microbiota can lead to further testing in order to get a
finite answer for bacterial vaginitis investigations.
This webinar will discuss the increased
sensitivity and specificity required for vaginal microbiota and pathogen
investigations. It will also review the role of both pathogenic and commensal
microbiota involved in urogenital infections, and identify the methods
to detect a broad range of vaginal microbiota from a single sample
quickly, and
efficiently.
This webinar will:
•
Review the role of both pathogenic and commensal microbiota
involved in urogenital infections
•
Identify the methods to detect a broad range of vaginal
microbiota from a single sample quickly, and cost effectively
•
Discuss the practical application of the detection of a
broad range of vaginal microbiota from a single sample
|
Presenters:
 |
Don Stalons, PhD
Director, Clinical Laboratory, Diatherix |
 |
Doug Rains
CSO of Quantigen Laboratory in Fishers, IN |
 |
Jeffrey Shaman, PhD
Director of Business Dev.
Coriell Life Sciences |
|
Case Studies in Vaginitis
Live Event: Friday, March 31, 2017 |
2:00 - 3:00 PM EST
PACE® credit available
until September 31, 2017 | Florida Laboratory CE Credit
available |
 |
Vaginitis is one of the most common gynecologic disorders seen in
primary care It is a disorder that accounts for 10 million office visits
and up to 7 percent of visits made to gynecologists. Although generally
not regarded as a serious condition, it nevertheless has significant
consequences in terms of pain and discomfort, days loss from work and
school, sexual functioning, and altered self-esteem. In addition, over
one billion dollars a year are spent on OTC medications and physician
visits for this diagnosis.
This webinar will provide clinicians with a practical diagnostic
approach to the patient presenting to the office with a vaginal
discharge. In addition to helping the clinicians differentiate normal
from abnormal, the webinar will also illustrate how integration of clues
from the history and physical findings with skillful use of the office
laboratory is essential for making an accurate diagnosis. This webinar
will also address current challenges in diagnosing trichomonas and
candida infections and review the effective management of common vaginal
infections.
This webinar will:
•
Describe a differential diagnosis of the patient presenting with
a vaginal discharge.
•
Analyze the role of the office laboratory in diagnosing
vaginitis.
•
Identify the three most common causes of vaginitis and discuss
the effective management of each.
|
Presenter:
Martin Quan, MD
Professor of Clinical Family Medicine
David Geffen School of Medicine at UCLA

Dr. Quan is Professor of Clinical Family
Medicine and Vice Chair for Academic Affairs, Department of Family
Medicine, David Geffen School of Medicine at UCLA and is also Director,
Office of Continuing Medical Education. He also serves as Senior
Advisor to the President of the American Board of Family Medicine. He is
a member of the Education Advisory Board and consultant to the Committee
on Continued Professional Development of the California Academy of
Family Physicians and a member of the Kidney Learning System Advisory
Board of the National Kidney Foundation. |
Tissue Archiving: Reality, Recommendations and Best Practices
Live Event: Thursday, January 26, 2017
| 1:00 - 2:00 PM EST
PACE® credit available
until January 26, 2018 | Florida Laboratory CE Credit
available |
  |
In today’s busy Pathology laboratories, more is being expected with
fewer resources. Yet, archiving tissue paraffin blocks, retrieving them
when necessary and then re-archiving them back into their original filed
positions utilizes manpower resources. An estimated 3000 manual work
hours are spent annually for a laboratory that processes 100,000 tissue
blocks per year.1
More importantly, the traceability and accountability of tissue blocks
are critical components to patient management. The risk of delay of
diagnosis when tissue blocks go missing can lead to anxiety for the
patient and the laboratory staff. In addition, lost tissue blocks can
result in even more serious issues including risk of litigation and
harmed reputation. As serious as lost patient diagnostic pathology
slides can be, lost paraffin blocks are even more significant since any
hope of retrieving a viable patient sample is lost forever.2
The purpose of this webinar is to review tissue block archiving
guidelines in the US and other countries throughout Europe. It will
review the past and current practice for archiving tissue blocks at Dr.
Costes-Martineau’s laboratory at Montpellier University Teaching
Hospital. And lastly, it will offer recommendations on best practices
towards achieving overall improvement in tissue block archiving
practices.
1Montpellier
University Teaching Hospital, Montpellier, France
2Testing Biopsy & Cytology Specimens for Cancer,
www.Cancer.org
This webinar will:
•
Review tissue block archiving guidelines in the US and discuss
how these regulations compare to those in other countries throughout
Europe.
•
Examine how one laboratory achieved time-savings while improving
compliance with their tissue block archiving system.
•
Identify best practices towards improving your laboratory’s
efficiency in tissue block archiving.
|
Presenter:
Pr. Valérie Costes-Martineau, MD
Montpellier University Teaching Hospital, Montpellier, France

Dr. Costes-Martineau is Professor of Medicine at University Montpellier.
She is the head of both the Department of Biopathology and of the
Department of Biobanking at Montpellier University Teaching Hospital in
France. Professor Costes-Martineau's main focus is Head and Neck (HN)
Pathology. She is a member of the Scientific Board of the network for
rare HN cancers which is granted by INCA, and in charge of HN Pathology
Teaching organized by the Pathology French Society. She is also the
president of the French HN Pathology society. Professor Costes-Martineau
is the author of over 100 articles in peer reviewed scientific journals. |
Molecular In Minutes: The Value
of Molecular Testing for Infectious Disease
Live Event:
Wednesday, December 14, 2016
| 2:00 - 3:00 PM EST
PACE® credit available
until June 14, 2017 | Florida Laboratory CE Credit
available |
  |
Overuse of antibiotics is a significant global crisis. While physicians
often prescribe treatment empirically rather than wait for diagnostic
results, hospitals are faced with a financial burden for antibiotic
resistant infections and C. difficile rates. As laboratories
increasingly have the ability to deliver faster results, they can now
also have more impact on the treatment patients receive. By helping to
ensure that patients are placed on the most appropriate therapy,
complications like C. difficile infection and the resulting increased
length of stay can be better managed.
This webinar will:
•
Define the need for changing antibiotic prescribing habits at
point-of-care
•
Discuss newer technologies that amplify nucleic acid
•
Explain how these technologies can apply to specific disease
states
|
This webinar is sponsored by |
 |
|
Presenter:
Norman Moore, PhD
Director of Scientific Affairs for Infectious Disease, Alere

Dr. Moore received his bachelor’s degree in
biology and philosophy from Dartmouth College and his Ph.D. in
microbiology from the University of New Hampshire. He developed the
first ever rapid tests for Legionella and S. pneumoniae, both of which
are now recommended by the Infectious Disease Society of America for use
in severe pneumonia cases, among other assays. Dr. Moore currently has
six patents and numerous publications and presentations.
|
Rheumatoid Arthritis Diagnosis: Avoiding CCP False Positives
Live Event: Monday, October 24, 2016 | 11:00
AM - 12:00 PM EDT
PACE® credit available
until April 24, 2017 | Florida Laboratory CE Credit
available |
  |
Rheumatoid arthritis (RA) is the second most
common autoimmune disease, just behind autoimmune thyroid diseases, and
more common than RA disease, antiphospholipid syndrome and autoimmune
liver diseases. RA is a chronic, systemic inflammatory disorder
affecting approximately 1.3 to 2.6 million (0.5 - 1%) adults, and
294,000 children in the US1. In nearby Canada, researchers
found an incidence of 2 and 5 cases per 1000 residents, with prevalence
in women over 45 close
to 1%2.
The cause of RA is unknown and there is no cure, however early treatment
can help prevent irreversible joint damage, premature death, disability,
and raise the patient’s quality of life3. In many geographic
regions access to specialty care is limited. The American Academy of
Pediatrics (AAP) considers access to rheumatologists, and particularly,
pediatric rheumatologists as one of their top 8 concerns.
Expanded management of patients is challenging in that the diagnosis is
formed using established medical guidance criteria including the
combination of physical exam, serologic testing and imaging.
Understanding serologic test selection and interpretation can improve
qualified referrals to help meet demand for specialty care. This webinar
will address evidence-based approaches described in the American college
of Rheumatology Guidelines for the diagnosis and management of
Rheumatoid Arthritis.
This webinar will:
•
Review evidence-based approaches described in the American
college of Rheumatology Guidelines for the diagnosis and management of
Rheumatoid Arthritis
•
Discuss the importance of specificity in test selection, and
optimal usage of two recommended serologic markers for RA, Anti-CCP and
Rheumatoid Factor IgM
•
Analyze how test efficacy and disease prevalence impact result
accuracy, and timely consultation or referral to a rheumatologist for
patients in whom there is a high index of suspicion of RA
1
Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence
of arthritis and other rheumatic conditions in the United States. Part
I. Arthritis Rheum. 2008 Jan;58(1):15-25. doi: 10.1002/art.23177.
2 Broten L, Aviña-Zubieta JA, Lacaille D, et. Al. Systemic
autoimmune rheumatic disease prevalence in Canada: updated analyses
across 7 provinces.JRheumatol. 2014 Apr;41(4):673-9.
doi:10.3899/jrheum.130667.Epub 2014 Mar 1.
3 Herold M. Rheumatoid Arthritis. In: Shoenfeld Y and Meroni
PL, ed. The General Practice Guide To Autoimmune Diseases. Lengerich,
Germany: Pabst Science Publishers; 2012:63-71.
|
Presenter:
Teresa Tarrant, MD
Assistant Professor of Medicine
Duke University School of Medicine Durham, North Carolina

Dr. Tarrant is a clinical immunologist, board certified in allergy,
immunology and rheumatology. She specializes in diseases of and related
to rheumatoid arthritis, Sjögrens syndrome, inflammatory eye disease,
CVID, and immunodeficiency in aging. In addition to her active medical
practice, over the last 10 years, Dr. Tarrant has held two other major
roles in her daily work; first as a medical liaison, where she assists
in the evaluation and selection of immunoassays, including authoring or
co-authoring peer-reviewed scientific articles of their evaluations, and
secondly as an associate professor of medicine. |
Comparing Biomarkers used in Infection, Sepsis, and Septic
Shock:
What is the Role of Procalcitonin?
Live Event: Tuesday, September 13, 2016 | 2:00 -
3:00 PM EDT
PACE® credit available
until March 13, 2017 | Florida Laboratory CE Credit
available |
  |
Sepsis is the 6th most common principal diagnosis affecting 1 in 23
inpatients. The in-hospital mortality rate due to sepsis is 16%, which
is nearly 8 times higher than the average inpatient mortality rate, and
adversely impacts clinical outcomes for hospitals.
Septicemia is the second highest 30-day Medicare readmission diagnoses,
resulting in 92,900 readmissions. Sepsis is the most expensive inpatient
diagnosis with over $23B in aggregate hospital costs, accounting for
5.2% of all costs, but only 2.8% of discharges.
This webinar will help participants assess whether their current
biomarker choices provide their clinicians with optimal clinical
effectiveness. Procalcitonin (PCT) is a biomarker of the host's response
to a systemic bacterial infection. The webinar will illustrate how PCT
provides rapid insight on the severity of bacterial infection, the risk
of progression to sepsis, and the risk of mortality.
This webinar will also review currently available biomarkers used for
infectious disease diagnosis, sepsis, and septic shock.
This webinar will:
• Review currently available biomarkers used for infectious disease
diagnosis, sepsis and septic shock
• Compare and contrast common biomarkers to determine which marker or
group of markers can provide clinicians with effective clinical
information
• Discuss the role of Procalcitonin (PCT) in sepsis management
|
Presenter:
Mike Broyles, BSPharm, PharmD,
Dir. Pharmacy and Laboratory Services
Five Rivers Medical Center, AR

Dr. Broyles is a Doctorate Prepared Pharmacist with 25 years of
experience as a Hospital Pharmacy Director providing patients with
current concepts in the clinical use of drugs. As the pharmacy advisory
chairman for a large IDN, Dr. Broyles helps to develop and implement
clinical initiatives. He consults for several IDN’s, Alaris, Cardinal
Health, Carefusion, bioMerieux, ICNet, independently serving both small
and large hospitals. |
The
Impact of Point-of-Care Hemoglobin Testing on Patient Blood Management
Live Event: Monday, August 22, 2016 | 2:00 -
3:00 PM EDT
PACE® credit available
until February 22, 2017 | Florida Laboratory CE Credit
available |
  |
Patient Blood Management (PBM) is an emerging clinical concept designed
to reduce unnecessary, excessive and avoidable blood transfusions.
Interest in PBM has grown rapidly throughout the world as new evidence
demonstrates a strong association between transfusion and a variety of
healthcare care complications (infections, pulmonary injury, and
mortality). Reducing transfusion exposure in hospitals has the dual
benefit of significantly reducing costs while improving safety and
outcomes.
PBM programs often utilize a variety of resources and technologies to
optimize blood management, including point-of-care testing.
Point-of-care Hemoglobin testing has been widely used in hospitals and
published in the literature as an evidence based strategy to support
transfusion management. This webinar will focus on practical
applications of POCT Hgb to improve the recognition and management of
anemia, support the paradigm shift of RBC transfusion as single units
with reassessment, and optimize transfusion decision making in the
anemic or bleeding patient.
This webinar will:
• Describe how optimal transfusion practice and patient blood
management can result in reduced health care costs and improved patient
outcomes
• Define how point-of-care Hemoglobin testing can improve
recognition/management of anemia and transfusion decision making in the
bleeding patient
• Examine the paradigm shift of RBC transfusion as single units with
reassessment
Click here to learn more about Fisher HealthCare's solutions for Patient
Blood Management. |
Presenter:
Joseph Thomas, BSN, RN
Regional Director, Blood Management - Accumen

Joseph Thomas is a registered nurse and currently serves as Regional
Director of Patient Blood Management (PBM) for Accumen. Over the past 14
years Mr. Thomas has worked with over 125 hospitals to improve blood
management and patient outcomes. Over this time he has educated and
mentored thousands of physicians and nurses on transfusion and blood
management related topics. Mr. Thomas is also a nationally recognized
speaker and a published author in the field of blood management and
transfusion safety. |
Epidemiology,
Diagnosis, and Prevention of Clostridium difficile
Infection
Live Event: Wednesday, May 18, 2016 | 2:00 -
3:00 PM EDT
PACE® credit available
until November 18, 2016 | Florida Laboratory CE Credit
available |
  |
The incidence and severity
of Clostridium difficile infection (CDI) has increased
dramatically since 2000. In 2011, there were 453,000 CDI cases in the US
associated with over 29,000 deaths. The clinical microbiology laboratory
plays a critical role in identifying patients who have CDI, and
therefore also the initiation of preventive measures. At the end of the
webinar, the participant will understand how CDI impacts patients, how
to optimize CDI diagnosis, and how to prevent CDI.
This webinar will:
• Analyze the importance of C. difficile infection on patient
outcomes
• Identify the advantages and disadvantages of C. difficile
diagnostic assays
• Describe the role of the microbiology laboratory in the prevention of
C. difficile infection
Click here to learn more about Fisher HealthCare's solutions for Clostridium difficile testing.
|
This webinar is sponsored by |
 |
|
Presenter:
Erik R. Dubberke, MD, MSPH
Associate Professor of Medicine, Washington University School of
Medicine

Dr. Dubberke is an Associate Professor of Medicine at Washington
University School of Medicine in St. Louis, where he has been a faculty
member in the Division of Infectious Diseases since 2005. His main
research interests are in the epidemiology, diagnosis, treatment, and
prevention of Clostridium difficile infection (CDI).
|
Cryptosporidium and Giardia
Testing
Live Event: Tuesday, May 3, 2016
| 2:00 - 3:00 PM
PACE® credit available
until November 3, 2016 | Florida Laboratory CE Credit
available |
|
In the United
States, CDC estimates approximately 2 million annual cases of Giardia
and Cryptosporidium combined. These numbers are likely underestimates of
true infections due to the challenges of traditional diagnostic methods.
The current gold standard for Giardia and Cryptosporidium detection is
conventional microscopy, which is time consuming, requires expert
technical skills, and is relatively insensitive. Additionally,
Cryptosporidium diagnosis requires special staining methods that may or
may not be considered by the ordering physician, potentially leading to
missed diagnoses of cryptosporidiosis.
Manufacturers are continually improving upon diagnostic assays to
enhance identification and detection of Giardia and Cryptosporidium,
resulting in a more accurate number of cases reported, better diagnosis
of true infections, and improved patient care.
This webinar will:
• Discuss giardiasis and cryptosporidiosis disease and epidemiology
• Identify the strengths and weaknesses of gold standard methods
• Describe current diagnostic methods for detecting Giardia and
Cryptosporidium in clinical specimens
• Review the impact these advanced methodologies have on improving
diagnosis
Click here to learn more about Fisher HealthCare's Cryptosporidium and
Giardia Testing solutions.
| This webinar is sponsored by |
 |
|
Presenter:
Shelley Miller, PhD, D (ABMM)
Clinical Instructor, UCLA

Dr. Shelley Miller completed a medical microbiology and public health
postdoctoral fellowship at UCLA and became board certified by the
American Board for Medical Microbiology. She is currently a
Clinical Instructor at the UCLA Clinical Microbiology Lab where she has
clinical teaching responsibilities and also helps oversee clinical trial
studies being conducted in the lab. |
Minutes vs. Days:
Rapid Diagnosis of Group A Strep
Live Event: March 30, 2016 | 3:00
- 4:00 PM EDT
PACE® credit available
until September 30, 2016 | Florida Laboratory CE Credit
available |
  |
Medical
providers now have a number of new technologies available for the rapid
diagnosis of strep pharyngitis. Dr. Schuman will present an overview of
strep pharyngitis, signs, symptoms and complications with an emphasis on
expediting diagnosis in the medical office. The role of the strep score
with be reviewed and discussed regarding its clinical utility.
Recommendations will be made for improving your current diagnostic
technology.
This webinar will:
• Discuss clinical features of strep pharyngitis
• Analyze the utility of the modified strep score in diagnosing strep
pharyngitis
• Identify the advantages and disadvantages of current "high tech" point
of care rapid strep tests
Click here to learn more about Fisher HealthCare's Strep A solutions.
| This webinar is sponsored by |
 |
|
Presenter:
Dr. Andrew J. Schuman
Geisel School of Medicine

Andrew J. Schuman is Clinical Assistant Professor of
Pediatrics, Geisel School of Medicine at Dartmouth. He has been writing
about office technology and medical practice in Contemporary Pediatrics
for 28 years, and he is now on the Editorial Advisory Board of the
publication. |
A Healthy Response to
Unhealthy Food: Diagnostic Testing for Wheat-Related Disorders
Live Event: Monday, November 9, 2015
| 2:00 - 3:00 PM EST
PACE® credit available
until May 9, 2016 | Florida Laboratory CE Credit
available |
  |
Researchers have found that there is a
spectrum of gluten-related disorders, which includes diseases and
conditions that result from the ingestion of gluten, a protein found in
wheat, barley and rye. This session will summarize our current knowledge
about the three main forms of reactions to wheat and its byproducts
including gluten: allergic (wheat allergy), autoimmune (celiac disease)
and intolerance (gluten sensitivity), and outline pathogenic, clinical
and epidemiological differences.
This webinar will:
• Distinguish between wheat allergy, celiac disease and non-celiac
gluten sensitivity
• Analyze and define testing requirements to aid in the diagnosis of
wheat allergy and gluten related disorders
• Advocate for accurate and timely diagnosis to improve patients quality
of life
• Review literature to better understand the presentation of symptom,
challenges of diagnosis and treatment options
Click here to learn more about Fisher HealthCare's solutions for Celiac
Disease testing |
Presenter:
Stefano Guandalini, MD
University of Chicago Celiac Disease Ctr
Stefano Guandalini, MD, is an internationally recognized expert on
celiac disease, a digestive disease that damages the small intestine and
interferes with absorption of nutrients from food. He is also known for
his expertise in the research and treatment of other diarrheal diseases
in children. Dr. Guandalini is the president of the North American
Society for the Study of Celiac Disease, and has been ranked among
America’s "Best Doctors" since 2008. |
The Unseen Threat: Diabetes
and the Cardiorenal Syndrome
Live Event: Wednesday, Oct 21, 2015 | 2:00 -
3:00 PM EDT
PACE® credit available
until April 21, 2016 | Florida Laboratory CE Credit
available |
  |
The statistics are staggering. Nearly 29.1 million children and adults
are living with diabetes in the U.S., and nearly 8.1 million (27.8%)
Americans remain undiagnosed.1 Additionally, approximately 26 million
Americans have kidney disease and are unaware of their condition.2
Diabetes poses a significant clinical burden to patients. Left
untreated, serious complications can occur including heart disease,
stroke, kidney failure, blindness, lower-limb amputation and pregnancy
complications. According to the International Journal of Nephrology
(IJN)3, Cardiorenal Syndrome (CRS) is the umbrella term used to describe
clinical conditions in which cardiac and renal dysfunctions coexist
whereby “acute or chronic dysfunction in one organ may induce acute or
chronic dysfunction of the other.” A number of laboratory tests such as
HbA1c, BNP, NT-proBNP, Albumin and Creatinine can assist clinicians in
the management of this syndrome.
Given the continued rise of diabetes in the U.S., healthcare
professionals need to be well-informed about Cardiorenal Syndrome, its
pathophysiology, its connection with diabetes and understand the latest
recommended guidelines for diagnosis and treatment.
This webinar will:
• Discuss the nature of Cardiorenal Syndrome and its pathophysiology
connection with diabetes
• Review the prevalence of diabetes and kidney diseases in the U.S.
• Examine the latest guidelines from leading research groups on this
topic
• Apply learnings to Cardiorenal Syndrome case studies
Click here to learn more about Fisher HealthCare's Diabetes Testing solutions.
|
Presenter:
Nancy Haley PhD

Dr. Haley has published over 150 articles in peer reviewed journals and
has written over 15 chapters in educational texts. She has lectured at
several international meetings on cardiology and cancer risk and has
appeared on Good Morning America, the Late Show with David Letterman,
and the ABC World News with Peter Jennings. |
Shiga Toxin: A
Public Health Threat
Live Event: Tuesday, July 14, 2015 | 2:00 -
3:00 PM EDT
PACE® credit available
until January 13, 2016 | Florida Laboratory CE Credit
available |
  |
Each year,
there are roughly 211-375 million diarrhea cases in the United States
leading to 73 million physician consultations, 3100 deaths, and $25
billion in healthcare costs. While the CDC estimates that 265,000 cases
occur each year due to Shiga Toxin producing E. coli (STEC), it is still
significantly underdiagnosed because appropriate diagnostic tests are
often not performed. STEC can not only cause bloody diarrhea, but has
complications like hemolytic uremic syndrome (HUS) in children and
thrombotic thrombocytopenic purpura in adults.
When a patient presents with symptoms of STEC, rapid diagnosis is key to
both improving the likelihood of a positive outcome and to helping
contain any further contamination. The test must also be accurate
because the wrong antibiotic treatment can actually exacerbate the
toxin.
This webinar will:
• Discuss the clinical significance of Shiga Toxin producing E. coli
(STEC) and its effect on public health
• Demonstrate how STEC can be transmitted and what foods are at highest
risk.
• Review the ways in which STEC causes significant illness, especially
in younger children
• Analyze the need for and how to test and treat for STEC.
Click here to learn more about Fisher HealthCare's Antimicrobial Stewardship solutions.
| This webinar is sponsored by |
 |
|
Presenter:
Norman Moore, PhD
Alere

Dr. Moore received dual degrees in Biology and Philosophy from Dartmouth
College and a PhD in Microbiology from the University of New Hampshire.
While at Digene Diagnostics, he developed tests for HPV, the etiological
agent for cervical cancer. While at Gene Trak Systems, Dr. Moore
developed diagnostics for food pathogens. Dr. Moore later joined Binax
where he developed the first ever rapid tests for Legionnaires ’
disease, S. pneumoniae in urine, and many other tests. Dr. Moore is
responsible for Scientific Affairs for infectious diseases at Alere.
|
|
Fisher Healthcare is approved as a provider of continuing education
programs in the
clinical laboratory sciences by the ASCLS P.A.C.E.® Program. |
| More
Educational Resources |
 |
Fisher Healthcare's commitment to
education extends to our sponsorship of many Point of Care
Group webinars. These webinars are produced by Whitehat Communications and free
to the point of care and laboratory community. You can register for
upcoming webinars and view the recorded sessions for 2018 here:
Click here to register
for any of the 2019 Point of Care group webinars
|
 |
| |
|
|
© 2021 | Whitehat
Communications, a division of Martek Inc. |
























































 Alain
Rico
Alain
Rico Matt
Osentoski
Matt
Osentoski


 Barbara
Van Der Pol, PhD, MPH
Barbara
Van Der Pol, PhD, MPH Obiageli
(Oby) Okafor, MD, DrPH
Obiageli
(Oby) Okafor, MD, DrPH
 Bruce
Lobaugh, Ph.D., HCLD(ABB)
Bruce
Lobaugh, Ph.D., HCLD(ABB)  Michael
Green MD, MS
Michael
Green MD, MS
 Denise
Pernal, HT (ASCP)
Denise
Pernal, HT (ASCP) Elizabeth
“Buffy” Pancake, MPM, HT (ASCP)
Elizabeth
“Buffy” Pancake, MPM, HT (ASCP)
 Matthew Binnicker, PhD
Matthew Binnicker, PhD Paul Drain, MD, MPH, FIDSA
Paul Drain, MD, MPH, FIDSA  Giovanni
Insuasti, MD
Giovanni
Insuasti, MD  Andrew
Hutchison
Andrew
Hutchison  Manoj Gandhi, MD, PhD
Manoj Gandhi, MD, PhD Vijay
Singh, MS, PhD
Vijay
Singh, MS, PhD Steven
Giglio PhD
Steven
Giglio PhD Rhys
Hill
Rhys
Hill
.jpg)

 Matthew
Faron, PhD
Matthew
Faron, PhD Omai
Garner PhD, D(ABMM)
Omai
Garner PhD, D(ABMM)
 Glen
Hansen, PhD, FCCM, D(ABMM)
Glen
Hansen, PhD, FCCM, D(ABMM) Jacqueline
Getty, MLS (ASCP)
Jacqueline
Getty, MLS (ASCP) Joseph
Mann, MSN, FNP-C, Global Medical Science Liaison
Joseph
Mann, MSN, FNP-C, Global Medical Science Liaison Megan
Wimmer, Associate Director
Megan
Wimmer, Associate Director


 Alexander
Craig Mackinnon, MD, PhD
Alexander
Craig Mackinnon, MD, PhD


 Donna
M. Wolk, MHA, Ph.D., D(ABMM), Geisinger Diagnostic Medicine
Institute, Geisinger Commonwealth School of Medicine
Donna
M. Wolk, MHA, Ph.D., D(ABMM), Geisinger Diagnostic Medicine
Institute, Geisinger Commonwealth School of Medicine Jelena
Feenstra, Ph.D.
Jelena
Feenstra, Ph.D.







 David
Baunoch, PhD
David
Baunoch, PhD Trisha
Lauterbach, MSA, MLS (ASCP), CHT (ASHI)
Trisha
Lauterbach, MSA, MLS (ASCP), CHT (ASHI)

























 Timothy
Triche, MD, PhD, Pathologist; Co-Director, Center for
Personalized Medicine Program (CPM) Professor of Pathology and
Pediatrics, USC Keck School of Medicine
Timothy
Triche, MD, PhD, Pathologist; Co-Director, Center for
Personalized Medicine Program (CPM) Professor of Pathology and
Pediatrics, USC Keck School of Medicine Mickey
Williams, PhD
Mickey
Williams, PhD Barbara
A. Conley, MD Special Volunteer / Contractor, National
Cancer Institute
Barbara
A. Conley, MD Special Volunteer / Contractor, National
Cancer Institute